Pretty Simple
Pretty Simple



Cancer often hides, with symptoms not appearing until later stages. The earlier that cancer is diagnosed, the greater the chance of successful treatment and survival.
For many when symptoms arise is can be late in the cancer!
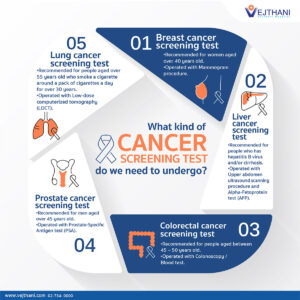
Currently, there are five cancers that are recommended for screening regularly in the U.S.:
- Mammographies test for breast cancer, typically in women ages 45 to 54.
- HPV tests and Pap tests screen for cervical cancer, typically in women ages 25 and up.
- Colonoscopies test for colorectal cancer in adults over age 45.
- Low-dose CT scans can be conducted on those who are at high risk for lung cancer if they’re former smokers or have had occupational hazard exposure.
- Prostate-specific antigen (PSA) tests screen for prostate cancer in men ages 55 and older.
Each of these screenings test for a specific kind of cancer and is done on a semi-regular basis. However, there isn’t currently a way to screen for more lethal cancers like pancreatic or ovarian cancer. These cancers aren’t usually caught until you start showing symptoms, and by then, the cancer has usually developed into stage III or stage IV and may have spread to other parts of your body.
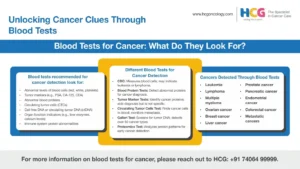
There is the Galleri test which is a multi -cancer early detection blood test that can identify over 50 types of cancer in asymptomatic adults aged 50 and older. It works by detecting tumor DNA in the blood stream, which can indicate the presence of cancer signals and help determine their likely origin in the body. The test is particularly effective for fast growing and aggressive cancers, which often require early detection. However, it is not a diagnostic tool and should be used in conjunction with other recommended screening methods. False positive and negatives can occur like other tests. The test is not recommended for individuals who are pregnant, younger than 22, or undergoing active cancer treatment.
The Galleri test invented by GRAIL, Inc. is an American biotechnology company based in Menlo Park, California founded in 2015 seeking to develop an early cancer screening test for people who do not have symptoms. As a startup it was a subsidiary of Illumina, which bought it outright in 2021.
In June 2021 Galleri launched their liquid biopsy, or multi-cancer early detection test, which they called Galleri test. In 2023 EU regulators ordered Grail to be spun-out from Illumina which was completed on June 24, 2024.
“Currently, we don’t detect the majority of cancers, including highly lethal ones, such as pancreatic or ovarian cancer, until symptoms are present,” says Dr. Klein, under Cleveland Clinic. “But Galleri can find those cancers at a time when they’re in an earlier stage and before symptoms appear.” Allan Klein, MD, is the Director of Cardiovascular Imaging Research, Director of the Center for the Diagnosis and Treatment of Pericardial Diseases, and a staff cardiologist in the Section of Cardiovascular Imaging, the Robert and Suzanne Tomsich Department of Cardiovascular Medicine, at the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute. He is also the Course Director for Diastology and Contrast Echo & New Technologies Courses—currently his 15th annual course. He is board-certified in internal medicine and cardiovascular medicine.
The Galleri test may present a far more efficient way of detecting cancer. Instead of searching for any one type of cancer, it screens an individual for multiple cancers. Its potential is to change the current screening process from screening for individual cancers to one where individuals are screened for multiple cancers with a single blood test.
Many cancers shed DNA into your bloodstream, known as cell-free DNA or circulating tumor DNA. This DNA is usually shed as cancer cells die. Using what’s called Next-Generation DNA Sequencing and machine learning, doctors are able to use a single blood draw (test) to look at various patterns in that DNA code and figure out two things: if a cancer signal is present, and from where the cancer likely started.
These patterns in your DNA are possible because of a biological process known as methylation. During this process, your body expresses certain genes but not others. You can picture it like a wall of light switches: for every switch you turn on, others might turn off, and different configurations produce different results. So, a skin cell will have one configuration, while a liver cell will have another. In the same way, healthy cells will have one configuration, while cancer cells will have a different one. And specific cancer types will have specific configurations different from other cancer types.
“It’s like fingerprints and how fingerprints tell the difference between two people,” explains Dr. Klein. “The methylation patterns are fingerprints that are characteristic of each kind of cancer. They look one way for lung cancer and different for colon cancer.”
If you take the Galleri test, you can have two possible results:
- No cancer signal detected means there’s no cancer DNA detected in your bloodstream.
- A cancer signal detected suggests you may have cancer.
If a cancer signal is detected, the Galleri test is able to identify which organ system the cancer is likely coming from with about 90% accuracy. If this happens, you would then have another test (like a blood test, CT scan or ultrasound of your kidneys, lungs, pancreas or other affected system) to verify the presence of cancer. Then, you can determine what treatment is right for you. The key here is that you’re catching cancer much earlier than you normally would have before you start showing physical symptoms.
Galleri can detect more than 50 types of cancer, including: Anal Cancer, Breast Cancer, Cervical Cancer, Esophageal Cancer, Kidney cancer, Leukemia, Liver Cancer, Mesothelioma Cancer, Oral Cancer, Pancreatic Cancer, Stomach and Uterine Cancer.
This is especially effective when you consider that some of these cancers are extremely rare and highly lethal. In the case of pancreatic cancer, which isn’t normally detected until stage III or stage IV and has a one-year survival rate of 5%, it means you can catch at least some cases much earlier than normal.
The Accuracy in the Galleri Test:
Depending on the test, traditional screening tests have a false-positive rate of 10% to 40%. Galleri has a 0.5% false-positive rate, which means it’s highly accurate.
“It finds 51.5% of cancers,” points out Dr. Klein. “If you look at the 12 cancers that account for two-thirds of all deaths in the U.S., it actually finds 67% of those.”
And it’s 89% effective in predicting where the cancer started.
Currently, the Galleri test is meant to be in addition to traditional screenings — so you should get screened for cancers as you normally would once you’ve reached the applicable age. But, Dr. Klein points out that as we develop more research and collect more data, it may be possible to test for most cancers in the future using a simple blood test without having to use screening tests of the past.
Part II This weekend!
 Pretty Simple
Pretty Simple