Symptoms of vocal damage include. Breathiness, huskiness, hoarseness, loss of vocal power, monotone, sore or tense throat, losing the voice, pitch breaks and easy vocal fatigue.
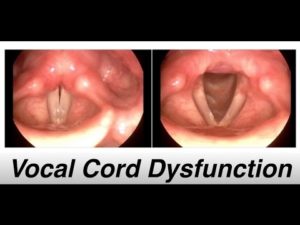
Vocal cord dysfunction or paradoxical vocal fold motion (PVFM) is an episodic condition that results when vocal cord movement is dysfunctional. We open our vocal cords when we breathe, and we close them when we speak, sing, swallow or lift heavy items. Vocal cord dysfunction describes what is occurring when our vocal cords close when we intended them to open to breathe. This incorrect vocal cord motion causes an abnormal narrowing of the voice box. The voice box narrowing leaves only a small opening for air to flow through the vocal cords, which can result in a sensation of difficulty moving air into or out of the lungs.
People who suffer PVFM episodes often have a very sensitive or reactive airway. Common triggers include:
- Acid reflux
- Exercise
- Postnasal drip or allergy to airborne particles
- Strong emotion
- Voice overuse
- Cough or fumes
Vocal cord dysfunction is sometimes misdiagnosed as asthma because the symptoms and triggers for PVFM and asthma can be similar. The difference between PVFM and asthma is that if you have asthma, medicines that open your breathing tubes (bronchodilators such as albuterol) will improve your breathing. If you have PVFM alone, the bronchodilator will likely not work.
To make it even more confusing, you may have both PVFM and asthma co-occurring.
What are the symptoms of vocal cord dysfunction?
- Throat or chest tightness
- Noisy inhalation
- Difficulty getting air “in”
- Feeling of throat closing
- Feeling of being “strangled”
- Intermittent shortness of breath
- Chronic cough
- Voice change/Inability to speak
Vocal Cord Dysfunction Treatment
Treatment for vocal cord dysfunction is often nonmedicinal and involves respiratory retraining therapy with a qualified speech-language pathologist. Therapy generally requires two to six 60-minute sessions. These sessions aim to:
- Identify and eliminate sources of chronic throat irritation.
- Identify and control triggers for PVFM episodes.
- Provide an exercise program to give patients better control over breathing, reduce the discomfort and fear that comes with being short of breath, and lessen PVFM episode frequency and duration.
- Include feedback to help the individual learn to relax the throat and keep the vocal cords apart when breathing.