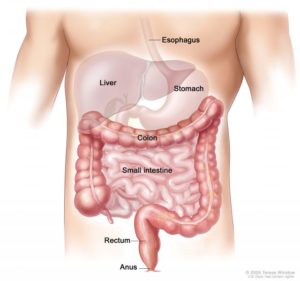
The GI tract starts at the mouth, to the esophagus, to the stomach, to the small intestines, than to the large intestines, than the rectum to the anus where we remove stool from the GI tract.
Know the cecum is a pouch-like passage that connects the colon to the ileum (the last part of the small intestine). If cancer develops in the cecum, it is treated like colon cancer.
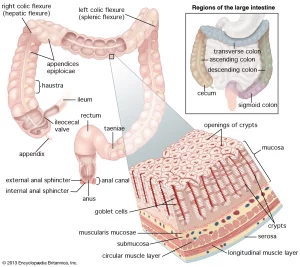
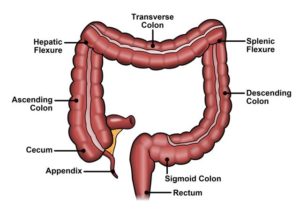
The entire colon is about 5 feet (150 cm) long, and is divided into five major segments. The rectum is the last anatomic segment before the anus, the last part of the GI tract is where the bowel movement comes out.
The ascending and descending colon are supported by peritoneal folds called mesentery.
The proximal colon is the ascending colon and the transverse colon together. The distal colon is the descending colon and the sigmoid colon together.
The right colon consists of the cecum, ascending colon, hepatic flexure and the right half of the transverse colon. The left colon consists of the left half of the transverse colon, splenic flexure, descending colon, and sigmoid.
The intestine is part of the digestive system. It is made up of the small intestine and the large intestine. The colon and rectum are parts of the large intestine. The colon is a U-shaped tube made of muscle, found below the stomach. The rectum is a shorter tube connected to the colon. Together, the colon and rectum are about 2 metres (6.5 feet) long. They are surrounded by other organs including the spleen, liver, pancreas, bladder and reproductive organs.
The large intestine is made up of the cecum, colon, rectum and anus. The colon and rectum are held in the abdomen by folds of tissue called mesenteries.
The rectum is the lower part of the large intestine that connects to the sigmoid colon. It is about 15 cm (6 in) long. It receives waste from the colon and stores it until it passes out of the body through the anus.
The anus is the opening at the lower end of the rectum through which stool is passed from the body.
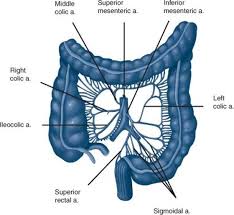
Blood Supply and Lymphatics
The superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA) provide blood supply to the colon. Communication between these two vessels happens via the marginal artery, which runs parallel to the length of the entire colon. The branches supplying specific portions of the bowel are as follows:
-
The cecum is supplied by the ileocolic artery, which is a terminal branch of the SMA. The ileocolic artery gives rise to the appendicular artery to supply the appendix.
-
The ascending colon and the right colic flexure are supplied by the ileocolic and right colic arteries, both branches of the SMA.
-
The arterial supply to the transverse colon is mostly from the middle colic artery, which is a branch of SMA. It may also receive blood supply from the anastomotic arcades between the right and left colic arteries, which collectively form the marginal artery.
-
The descending and sigmoid colon receive their blood supply from the left colic and sigmoid arteries, which are branches of the IMA. The transition of blood supply at the left colic flexure from the SMA to the IMA indicates the embryological transition from the midgut to hindgut that occurs at this point, respectively.
-
The rectum and anal canal are supplied by the superior rectal artery, which is a continuation of the IMA. They also receive supply from branches of the internal iliac arteries, the middle and inferior rectal arteries. Further, the inferior rectal artery is a branch of the internal pudendal artery.
Venous drainage usually accompanies arterial colonic supply. Ultimately, the inferior mesenteric vein (IMV) drains into the splenic vein, while the superior mesenteric vein (SMV) joins the splenic vein to form the hepatic portal vein. Lymphatics of the large intestine drain into the lymph nodes associated with the main vessels that supply them.
Nerves
The midgut-derived ascending colon and proximal two-thirds of the transverse colon receive parasympathetic, sympathetic, and sensory nerve supply from the superior mesenteric plexus.
The hindgut-derived structures, which include the distal one-third of the transverse colon, descending, and sigmoid colon, receive parasympathetic, sympathetic, and sensory nerve innervation from the inferior mesenteric plexus.
The key functions of the colon include the following:
-
Water and nutrient absorption
-
Vitamin absorption
-
Feces compaction
-
Potassium and chloride secretion
-
Moving waste material toward the rectum
Mechanism
Motility
The intestinal wall is made up of multiple layers. The 4 layers of the large intestine from the lumen outward are the mucosa, submucosa, muscular layer, and serosa. The muscular layer is made up of 2 layers of smooth muscle, the inner, circular layer, and the outer, longitudinal layer. These layers contribute to the motility of the large intestine. There are 2 types of motility present in the colon, haustral contraction and mass movement. Haustra are saccules in the colon that give it its segmented appearance. Haustral contraction is activated by the presence of chyme and serves to move food slowly to the next haustra, along with mixing the chyme to help with water absorption. Mass movements are stronger and serve to move the chyme to the rectum quickly.
Absorption of Water and Electrolytes
Absorption of water occurs by osmosis. Water diffuses in response to an osmotic gradient established by the absorption of electrolytes. Sodium is actively absorbed in the colon by sodium channels. Potassium is either absorbed or secreted depending on the concentration in the lumen. The electrochemical gradient created by the active absorption of sodium allows for this. Chloride ions are exchanged for bicarbonate ions across an electrochemical gradient.
Production/Absorption of Vitamins
The colon also plays a role in providing required vitamins through an environment that is conducive for bacterial cultivation. The colon houses trillions of bacteria that protect our gut and produce vitamins. The bacteria in the colon produce substantial amounts of vitamins by fermentation. Vitamin K and B vitamins, including biotin, are produced by the colonic bacteria. These vitamins are then absorbed into the blood. When dietary intake of these vitamins is low in an individual, the colon plays a significant role in minimizing vitamin disparity.
Now that we have reviewed the colon and rectum anatomy and physiology we will tomorrow start on colon cancer awareness for March.
Know cancer in the anal canal or anus is treated differently from colorectal cancer.
 the colon to rectum
the colon to rectum