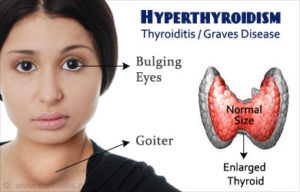
Hyperthyroidism, also called overactive thyroid, is when the thyroid gland makes more thyroid hormones than your body needs. The thyroid is a small, butterfly-shaped gland in the front of your neck. Thyroid hormones control the way the body uses energy, so they affect nearly every organ in your body, even the way your heart beats.
Possible Causes of Hyperthyroidism:
Hyperthyroidism has several causes, including Graves’ disease, thyroid nodules, and thyroiditis—inflammation of the thyroid. Rarely, hyperthyroidism is caused by a noncancerous tumor of the pituitary gland located at the base of the brain. Consuming too much iodine or taking too much thyroid hormone medicine also may raise your thyroid hormone levels.
-Graves’ disease
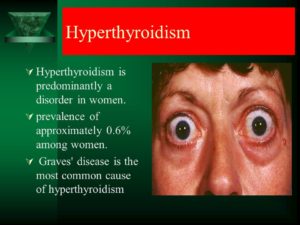
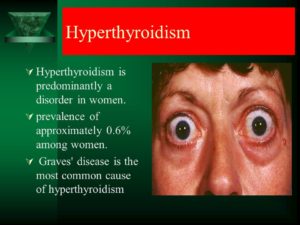
Graves’ disease is the most common cause of hyperthyroidism. Graves’ disease is an autoimmune disorder. With this disease, your immune system attacks the thyroid and causes it to make too much thyroid hormone.
-Overactive thyroid nodules
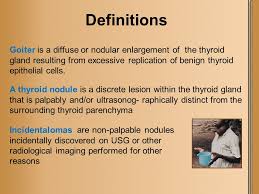
Thyroid nodules are lumps in your thyroid. Thyroid nodules are common and usually benign, meaning they are not cancerous. However, one or more nodules may become overactive and produce too much thyroid hormone. The presence of many overactive nodules occurs most often in older adults.
-Thyroiditis
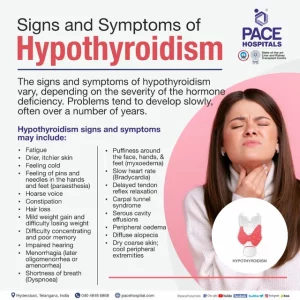
Thyroiditis is inflammation of your thyroid that causes stored thyroid hormone to leak out of your thyroid gland. The hyperthyroidism may last for up to 3 months, after which your thyroid may become underactive, a condition called hypothyroidism. The hypothyroidism usually lasts 12 to 18 months, but sometimes is permanent.
Several types of thyroiditis can cause hyperthyroidism and then cause hypothyroidism:
- Subacute thyroiditis. This condition involves a painfully inflamed and enlarged thyroid. Experts are not sure what causes subacute thyroiditis, but it may be related to an infection caused by a virus or bacteria.
- Postpartum thyroiditis. This type of thyroiditis develops after a woman gives birth.
- Silent thyroiditis. This type of thyroiditis is called “silent” because it is painless, even though your thyroid may be enlarged. Experts think silent thyroiditis is probably an autoimmune condition.
-Too much iodine
Your thyroid uses iodine to make thyroid hormone. The amount of iodine you consume affects the amount of thyroid hormone your thyroid makes. In some people, consuming large amounts of iodine may cause the thyroid to make too much thyroid hormone.
Some medicines and cough syrups may contain a lot of iodine. One example is the heart medicine amiodarone. Seaweed and seaweed-based supplements also contain a lot of iodine.
-Too much thyroid hormone medicine:
Some people who take thyroid hormone medicine for hypothyroidism may take too much. If you take thyroid hormone medicine, you should see your doctor at least once a year to have your thyroid hormone levels checked. You may need to adjust your dose if your thyroid hormone level is too high.
Some other medicines may also interact with thyroid hormone medicine to raise hormone levels. If you take thyroid hormone medicine, ask your doctor about interactions when starting new medicines
– A noncancerous tumor of the pituitary gland causing too much release of the hormone for the thyroid to release T3 and T4.
This is done by the tumor causing the pituitary gland over release thyroid stimulating hormone-TSH. Thyrotropinomas are pituitary adenomas that occur in the thyrotropic cells of the pituitary gland and secrete thyroid-stimulating hormone, or TSH. TSH, in turn, triggers the thyroid gland to become overly active and produce too much thyroid hormone, a condition known as hyperthyroidism.
It can also cause a wide variety of signs and symptoms:
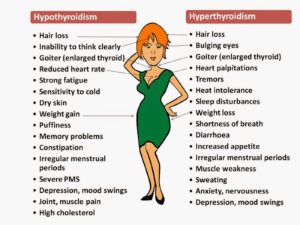
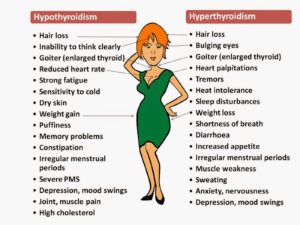
- Hyperthyroidism (overactive thyroid) is a condition in which your thyroid gland produces too much of the hormone thyroxine. Hyperthyroidism can accelerate your body’s metabolism significantly, causing sudden weight loss, a rapid or irregular heartbeat, sweating, and nervousness or irritability.
- Sudden weight loss, even when your appetite and the amount and type of food you eat remain the same or even increase
- Rapid heartbeat (tachycardia) — commonly more than 100 beats a minute — irregular heartbeat (arrhythmia) or pounding of your heart (palpitations)
- Increased appetite
- Nervousness, anxiety and irritability
- Tremor — usually a fine trembling in your hands and fingers
- Sweating
- Changes in menstrual patterns
- Increased sensitivity to heat
- Changes in bowel patterns, especially more frequent bowel movements
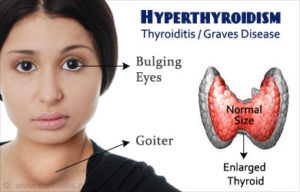
- An enlarged thyroid gland (goiter), which may appear as a swelling at the base of your neck
- Fatigue, muscle weakness
- Difficulty sleeping
- Skin thinning
- Fine, brittle hair
- Graves’ ophthalmopathy=An autoimmune disease that is frequently associated with hyperthyroidism.
- Sometimes an uncommon problem called Graves’ ophthalmopathy may affect your eyes, especially if you smoke. In this disorder, your eyeballs protrude beyond their normal protective orbits when the tissues and muscles behind your eyes swell. This pushes the eyeballs forward so far that they actually bulge out of their orbits. This can cause the front surface of your eyeballs to become very dry. Eye problems often improve without treatment.Older adults are more likely to have either no signs or symptoms or subtle ones, such as an increased heart rate, heat intolerance and a tendency to become tired during ordinary activities. Medications called beta blockers, which are used to treat high blood pressure and other conditions, can mask many of the signs of hyperthyroidism.
- Protruding eyeballs
- Red or swollen eyes
- Excessive tearing or discomfort in one or both eyes
- Light sensitivity, blurry or double vision, inflammation, or reduced eye movementIf you experience unexplained weight loss, a rapid heartbeat, unusual sweating, swelling at the base of your neck or other symptoms associated with hyperthyroidism, see your doctor. It’s important to completely describe the changes you’ve observed, because many signs and symptoms of hyperthyroidism may be associated with a number of other conditions.Causes: A number of conditions, including Graves’ disease, toxic adenoma, Plummer’s disease (toxic multi-nodular goiter) and thyroiditis, can cause hyperthyroidism.
When to be checked by the doctor:
Any of these signs or symptoms listed above you have that where never checked out by the doctor or if the new symptom (s) just recently started and where never diagnosed by the MD. If you’ve been treated for hyperthyroidism or currently are being treated, see your doctor regularly as advised so that he or she can monitor your condition. Also, if you are at a age that makes you in a age group that is more common to have this disease than have your MD check you out to see if you have the disease.
If hyperthyroidism isn’t treated, it can cause some serious health problems, including:
-an irregular heartbeat that can lead to blood clots, stroke, heart failure, and other heart-related problems
-an eye disease called Graves’ ophthalmopathy that can cause double vision, light sensitivity, and eye pain, and rarely can lead to vision loss
-thinning bones and osteoporosis
Risk factors:
Hyperthyroidism, particularly Graves’ disease, tends to run in families and is more common in women than in men. If another member of your family has a thyroid condition, talk with your doctor about what this may mean for your health with what you need to do.
Hyperthyroidism can be serious don’t ignore it, most people respond well once hyperthyroidism is diagnosed and treated. Hyperthyroidism can mimic other health problems, which may make it difficult for your doctor to diagnose.
Complications:
Untreated, hyperthyroidism can cause serious health problems, including
- an irregular heartbeat that can lead to blood clots, stroke, heart failure, and other heart-related problems
- an eye disease called Graves’ ophthalmopathy
- thinning bones, osteoporosis NIH external link, and muscle problems
- menstrual cycle and fertility issues