Archives
QUOTE FOR FRIDAY:
“Prothrombin deficiency is a disorder caused by a lack of a protein in the blood called prothrombin. It leads to problems with blood clotting (coagulation). Prothrombin is also known as factor II (factor two).
When you bleed, a series of reactions take place in the body that helps blood clots form. This process is called the coagulation cascade. It involves special proteins called coagulation, or clotting, factors. You may have a higher chance of excess bleeding if one or more of these factors are missing or are not functioning like they should.
Prothrombin, or factor II, is one such coagulation factor. Prothrombin deficiency runs in families (inherited) and is very rare. Both parents must have the gene to pass the disorder on to their children. A family history of a bleeding disorder can be a risk factor.
Prothrombin deficiency can also be due to another condition or use of certain medicines. This is called acquired prothrombin deficiency.”
Mount Sinai (https://www.mountsinai.org/health-library/diseases-conditions/factor-ii-deficiency)
Bleeding Disorder Month – Prothrombin Deficiency
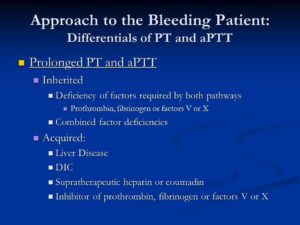
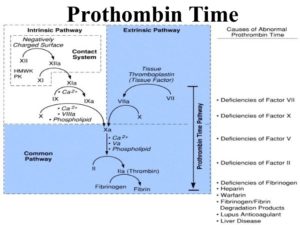
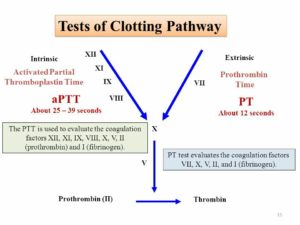
Prolonged PT and aPTT. Inherited. Deficiency of factors required by both pathways. Prothrombin, fibrinogen or factors V or X. Combined factor deficiencies. Acquired: Liver Disease. DIC. Supratherapeutic heparin or coumadin. Inhibitor of prothrombin, fibrinogen or factors V or X.
Prothrombin deficiency is a bleeding disorder that slows the blood clotting process. People with this condition often experience prolonged bleeding following an injury, surgery, or having a tooth pulled. … Women with prothrombin deficiency can have prolonged and sometimes abnormally heavy menstrual bleeding. This blood clotting factor II deficiency. Remember we have blood clotting factors that have to be present for the blood clotting factor but if one is lacking then bleeding can occur.
Practice Essentials
Clotting factor II, or prothrombin, is a vitamin K–dependent proenzyme that functions in the blood coagulation cascade. Factor II deficiency is a rare, inherited or acquired bleeding disorder disorder with an estimated incidence of one case per 2 million population. [1]
Inherited factor II deficiency is an autosomal recessive disorder that can manifest as hypoprothrombinemia, a decrease in the overall synthesis of prothrombin; or as dysprothrombinemia, the synthesis of dysfunctional prothrombin. [2, 3, 4] Homozygous individuals are generally asymptomatic and have functional prothrombin levels of 2-25%. However, symptomatic individuals may experience one or more of the following [1] :
-
Easy bruising
-
Epistaxis
-
Soft-tissue hemorrhage
-
Excessive postoperative bleeding
-
Menorrhagia
-
Muscle hematomas
-
Hemarthrosis
-
Intracranial bleeding
In true hypoprothrombinemia, immunologic assays correlate well with functional assays in that both reveal low prothrombin values. Heterozygous patients are generally asymptomatic and have prothrombin levels of 50% or greater on both immunologic and functional assays.
In dysprothrombinemia, only the functional assay for prothrombin returns significantly reduced values, whereas the immunologic assay reveals normal values. Acquired factor II deficiency can be caused by severe liver disease, vitamin K deficiency, anticoagulant drugs (eg, warfarin), or the presence of an antibody directed against the protein. [5]
Aside from the prothrombin deficiencies, another disorder of prothrombin is the prothrombin 20210a mutation. First reported in 1996 as a familial cause of venous thromboembolism, the prothrombin 20210a mutation results in increased levels of plasma prothrombin and a concurrent increased risk for the development of thrombosis. [6]
Prothrombin 20210a has an estimated prevalence of 2% in whites. [7, 8] The mutation is more prevalent in those of southern European descent than in those of northern European descent, and it is rarely seen in Asians or Africans. [7] A study of patients in Turkey revealed the presence of the prothrombin 20210a mutation in 0.7% of subjects. [9]
Individuals carrying the prothrombin 20210a mutation have a 2- to 3-fold increased risk for developing thrombosis. [6, 10] One case-control study found evidence of an increased risk of developing an ischemic cerebrovascular event in men aged younger than 60 years with the prothrombin 20210a mutation. [11] A study of cancer patients in the Netherlands found that the presence of the prothrombin 20210a mutation in these patients may increase the risk of venous thrombosis to a level greater than that attributable to the malignancy alone. [12]
The prothrombin 20210a mutation can be identified without DNA analysis and should be considered in any patient experiencing a thrombotic event without other risk factors. Treatment with oral anticoagulants is useful in preventing recurrence in patients with the mutation who have already experienced a thrombotic event. Additionally, women who are known to carry the mutation may want to avoid oral contraceptives because of the additional risk of thrombosis.
Laboratory studies for factor II deficiency include coagulation studies and clotting factor assays (see Workup). Coagulation study results are as follows:
-
Prothrombin time (PT) is prolonged
-
Activated partial thromboplastin time (aPTT) is prolonged
-
Bleeding time is within reference range
Treatment of factor II deficiency is aimed at restoring circulating factor II to levels sufficient for hemostasis. Levels greater than 30% of normal are usually adequate. Treatment measures include fresh frozen plasma (FFP), prothrombin complex concentrates (PCCs), and vitamin K. Additionally, in patients with acquired factor II deficiency, the underlying cause should be found and treated.
Frequency
Both congenital and acquired factor II deficiencies are rare. The prevalence of congenital factor II deficiency is approximately 1 per 1 to 2 million population. [41]
Mortality/Morbidity
Congenital factor II deficiency is a lifelong bleeding disorder. Death can result because of massive hemorrhage from relatively minor accidents or trauma. Hemorrhage can also occur as a result of surgery if precautions are not taken. Intracranial bleeding is another serious sequela of this disorder. Rarely, hemarthroses can occur. [2]
Myocardial infarction is a rare complication in young people, with coronary thrombosis due to hypercoagulable states being one cause. A heterozygote prothrombin gene mutation (G-20210-A) and protein S deficiency were described in a 19-year-old with a myocardial infarction with normal coronary arteries. [42]
Race- sex-, and age-related demographics
Factor II deficiency has no known racial or ethnic predilection. Males and females are affected equally. Patients with severe congenital factor II deficiency present early in life, whereas those with less severe forms can present at any age. Acquired forms can be observed in all age groups.
QUOTE FOR WEDNESDAY:
“Your kidneys, each just the size of a computer mouse, filter all the blood in your body every 30 minutes. They work hard to remove wastes, toxins, and excess fluid. They also help control blood pressure, stimulate production of red blood cells, keep your bones healthy, and regulate blood chemicals that are essential to life.
Kidneys that function properly are critical for maintaining good health, however, more than one in seven American adults are estimated to have chronic kidney disease (CKD).”
Centers for Disease Control and Prevention – CDC
(https://www.cdc.gov/kidneydisease/basics.html#:~:text=disease (CKD).-,About Chronic Kidney Disease,as heart disease and stroke.)
QUOTE FOR TUESDAY:
“Acute kidney injury (AKI) is where your kidneys suddenly stop working properly. It can range from minor loss of kidney function to complete kidney failure.
AKI normally happens as a complication of another serious illness. It’s not the result of a physical blow to the kidneys, as the name might suggest.
This type of kidney damage is usually seen in older people who are unwell with other conditions and the kidneys are also affected.
It’s essential that AKI is detected early and treated promptly.“
National Health Services-NHS (https://www.nhs.uk/conditions/acute-kidney-injury/)
QUOTE FOR MONDAY:
“The body takes nutrients from food and converts them to energy. After the body has taken the food components that it needs, waste products are left behind in the bowel and in the blood.
The kidney and urinary systems help the body to eliminate liquid waste called urea, and to keep chemicals, such as potassium and sodium, and water in balance. Urea is produced when foods containing protein, such as meat, poultry, and certain vegetables, are broken down in the body. Urea is carried in the bloodstream to the kidneys, where it is removed along with water and other wastes in the form of urine.”
John Hopkins Medicine (https://www.hopkinsmedicine.org/health/wellness-and-prevention/anatomy-of-the-urinary-system)
QUOTE FOR THE WEEKEND:
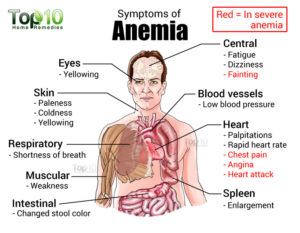
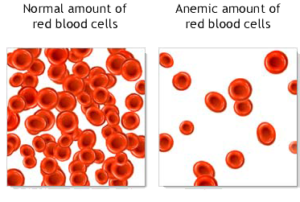
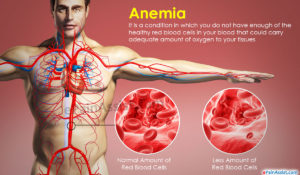
“Anemia is a problem of not having enough healthy red blood cells or hemoglobin to carry oxygen to the body’s tissues. Hemoglobin is a protein found in red cells that carries oxygen from the lungs to all other organs in the body. Having anemia can cause tiredness, weakness and shortness of breath.
There are many forms of anemia. Each has its own cause. Anemia can be short term or long term. It can range from mild to severe. Anemia can be a warning sign of serious illness.”
MAYO Clinic (https://www.mayoclinic.org/diseases-conditions/anemia/symptoms-causes/syc-20351360)
Anemia
Anemia develops when you don’t have enough robust, healthy red blood cells to carry oxygen throughout your body. The blood cells may lack enough hemoglobin, the protein that gives blood its red color. Anemia affects one in 10 teen girls and women. It also develops in men and children and is linked to some illnesses. Anemia is a condition that develops when your blood lacks enough healthy red blood cells or hemoglobin. Hemoglobin is a main part of red blood cells and binds oxygen. If you have too few or abnormal red blood cells, or your hemoglobin is abnormal or low, the cells in your body will not get enough oxygen. Symptoms of anemia — like fatigue — occur because organs aren’t getting what they need to function properly.
Anemia is the most common blood condition in the U.S. It affects about 3.5 million Americans. Women, young children, and people with chronic diseases are at increased risk of anemia.
There types of different anemia’s but today’s we’ll look more into is Iron Deficiency Anemia.
Iron deficiency anemia is a common type of anemia — a condition in which blood lacks adequate healthy red blood cells. Red blood cells carry oxygen to the body’s tissues.
As the name implies, iron deficiency anemia is due to insufficient iron. Without enough iron, your body can’t produce enough of a substance in red blood cells that enables them to carry oxygen (hemoglobin). As a result, iron deficiency anemia may leave you tired and short of breath.
You can usually correct iron deficiency anemia with iron supplementation. Sometimes additional tests or treatments for iron deficiency anemia are necessary, especially if your doctor suspects that you’re bleeding internally.
Initially, iron deficiency anemia can be so mild that it goes unnoticed. But as the body becomes more deficient in iron and anemia worsens, the signs and symptoms intensify.
Iron deficiency anemia symptoms may include:
- Extreme fatigue, Pale skin, Weakness, Shortness of breath, Chest pain, Frequent infections
- Headache, Dizziness or lightheadedness, Cold hands and feet, Inflammation or soreness of your tongue, Brittle nails, and Fast heartbeat.
- Unusual cravings for non-nutritive substances, such as ice, dirt or starch.
- Poor appetite, especially in infants and children with iron deficiency anemia.
- An uncomfortable tingling or crawling feeling in your legs (restless legs syndrome).
Causes of iron deficiency anemia include:
- Blood loss. Blood contains iron within red blood cells. So if you lose blood, you lose some iron. Women with heavy periods are at risk of iron deficiency anemia because they lose blood during menstruation. Slow, chronic blood loss within the body — such as from a peptic ulcer, a hiatal hernia, a colon polyp or colorectal cancer — can cause iron deficiency anemia. Gastrointestinal bleeding can result from regular use of some over-the-counter pain relievers, especially aspirin.
- A lack of iron in your diet. Your body regularly gets iron from the foods you eat. If you consume too little iron, over time your body can become iron deficient. Examples of iron-rich foods include meat, eggs, leafy green vegetables and iron-fortified foods. For proper growth and development, infants and children need iron from their diet, too.
- An inability to absorb iron. Iron from food is absorbed into your bloodstream in your small intestine. An intestinal disorder, such as celiac disease, which affects your intestine’s ability to absorb nutrients from digested food, can lead to iron deficiency anemia. If part of your small intestine has been bypassed or removed surgically, that may affect your ability to absorb iron and other nutrients.
- Without iron supplementation, iron deficiency anemia occurs in many pregnant women because their iron stores need to serve their own increased blood volume as well as be a source of hemoglobin for the growing fetus.
Those at risk for anemia:
Anemia is a common condition. It occurs in all age, racial, and ethnic groups. Both men and women can have anemia. However, women of childbearing age are at higher risk for the condition because of blood loss from menstruation.
Anemia can develop during pregnancy due to low levels of iron and folic acid (folate) and changes in the blood. During the first 6 months of pregnancy, the fluid portion of a woman’s blood (the plasma) increases faster than the number of red blood cells. This dilutes the blood and can lead to anemia.
During the first year of life, some babies are at risk for anemia because of iron deficiency. At-risk infants include those who are born too early and infants who are fed breast milk only or formula that isn’t fortified with iron. These infants can develop iron deficiency by 6 months of age.
Infants between 1 and 2 years of age also are at risk for anemia. They may not get enough iron in their diets, especially if they drink a lot of cow’s milk. Cow’s milk is low in the iron needed for growth.
Drinking too much cow’s milk may keep an infant or toddler from eating enough iron-rich foods or absorbing enough iron from foods.
Older adults also are at increased risk for anemia. Researchers continue to study how the condition affects older adults. Many of these people have other medical conditions as well.
Major Risk Factors for anemia:
- A diet that is low in iron, vitamins, or minerals
- Blood loss from surgery or an injury
- Long-term or serious illnesses, such as kidney disease, cancer, diabetes, rheumatoid arthritis, HIV/AIDS, inflammatory bowel disease (including Crohn’s disease), liver disease, heart failure, and thyroid disease
- Long-term infections
- A family history of inherited anemia, such as sickle cell anemia or thalassemia.
Complications of Anemia:
Some people who have anemia may have arrhythmias. Arrhythmias are problems with the rate or rhythm of the heartbeat. Over time, arrhythmias can damage your heart and possibly lead to heart failure.
Anemia also can damage other organs in your body because your blood can’t get enough oxygen to them.
Anemia can weaken people who have cancer or HIV/AIDS. This can make their treatments not work as well.
Anemia also can cause many other health problems. People who have kidney disease and anemia are more likely to have heart problems. With some types of anemia, too little fluid intake or too much loss of fluid in the blood and body can occur. Severe loss of fluid can be life threatening.
QUOTE FOR FRIDAY:
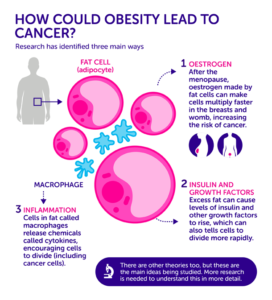
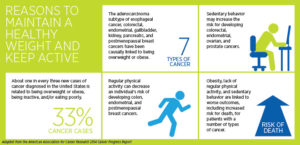
“Obesity has been linked to several common cancers including breast, colorectal, esophageal, kidney, gallbladder, uterine, pancreatic, and liver cancer. Obesity also increases the risk of dying from cancer and may influence the treatment choices. About 4–8% of all cancers are attributed to obesity. The underlying mechanism of obesity causing cancer is complex and is incompletely understood. Lifestyle changes that include diet, exercise, and behavior therapy are the mainstay of interventions. Drug therapy and weight reduction surgery result in a more rapid weight loss and may be used for a subgroup of cancer survivors with obesity.”
National Library of Medicine – NIH (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9857053/)
Supporting studies on the link between Obesity and Cancer.
LOOKING AT ACTUAL STUDIES SUPPORTING OBESITY&CANCER LINK
Take for example through the American Cancer Society they stated in an article 2006 that a substantial evidence from clinical trials has established that obesity significantly increases the risk for heart disease and diabetes. More recently, suspicions that obesity is linked to prostate cancer have been supported by a number of investigations, but the relationship has remained unclear. Now through a pair of new studies provides scientists with some important insights that may have an impact on how physicians manage their patients with prostate cancer.
The pair of studies show 2 significant studies relating how obesity links with prostate cancer, which were:
The implication is that prostate cancer patients who are obese should probably be followed more closely than patients with similar cancer characteristics who are not obese. That could include regular digital rectal exams, more frequent prostate-specific antigen (PSA) testing, and perhaps setting a lower PSA cutoff point as an indication of recurrence, Kane explained.
The greater risk associated with obesity may be related to technical issues, Kane said. For example, it’s more difficult for surgeons to perform a radical prostatectomy in obese patients. However, surgical challenges offer only a partial explanation. In studies where surgeons verified that they had removed all cancer cells during radical prostatectomy, obese patients were still more likely to experience a recurrence of the disease.
The second study, a multi-center trial coordinated at the Duke University School of Medicine in Durham, NC, found that obese men under the age of 63 tend to have larger prostates, which makes finding tumors more difficult. As a result, there’s a real danger of delayed diagnosis, which decreases the chances of a cure and puts patients at greater risk for dying of the disease. The findings appear in the Journal of Urology.
“It’s harder to find cancer in larger prostate glands,” explained Stephen J. Freedland, MD, assistant professor of urology and member of the Duke Prostate Center at the Duke University School of Medicine. “Consequently, our data suggest that we may be underdiagnosing cancers in younger obese men. That also means that the tumors we do pick up are likely to be at a more advanced stage and perhaps more aggressive, and therefore more difficult to treat.”
Let’s look at this at a broader aspect, not just pertaining to prostate cancer. This would be, “It’s not just patients with prostate cancer that studies like this should be directed toward,” Dr. Kane said. “Patients who are clearly at risk for developing the disease should also take notice of our findings. The central message is yet again that obesity has been identified as an important risk factor for a potentially deadly disease. For all of us, controlling our weight through diet and exercise is important, and we shouldn’t have blinders on and just think of prostate cancer. The number one risk of death for American men is heart disease, so anything we can do to reduce that risk that also reduces the risk for prostate cancer is useful.” Including it reduces risk for other cancers as well that are impacted by disease, it makes sense.
Obesity links to an increased risk of ovarian cancer.
Let’s look at this no: Atlanta 2009/01/05 -A new epidemiological study has found that among women who have never used menopausal hormone therapy, obese women are at an increased risk of developing ovarian cancer compared with women of normal weight. Published in the February 15, 2009 issue of CANCER, a peer-reviewed journal of the American Cancer Society, the research indicates that obesity may contribute to the development of ovarian cancer through a hormonal mechanism. Ovarian cancer is the most fatal of gynecologic malignancies, and has a 5-year survival rate of only 37 percent.
To investigate this issue, Dr. Michael F. Leitzmann of the National Cancer Institute and colleagues studied 94,525 U.S. women aged 50 to 71 years over a period of seven years. The researchers documented 303 ovarian cancer cases during this time and noted that among women who had never taken hormones after menopause, obesity was associated with an almost 80 percent higher risk of ovarian cancer. In contrast, no link between body weight and ovarian cancer was evident for women who had ever used menopausal hormone therapy.
According to Dr. Leitzmann, these findings support the hypothesis that obesity may enhance ovarian cancer risk in part through its hormonal effects. Excess body mass in postmenopausal women leads to an increased production of estrogen, which in turn may stimulate the growth of ovarian cells and play a role in the development of ovarian cancer.
In another study done 2003, American Cancer Society researchers analyzed data based on 900,000 American adults with obesity and cancer that they monitored for a total of 16 years. This is what they found in their landmark study:
1)The researchers found that the most obese women had a 62% increase in their risk of dying from cancer than women of normal weight; for obese men, the increase was 52%. The wide range of tumor types included colorectal, liver, gallbladder, pancreas, esophageal, kidney, prostate, breast, uterine, endometrial, and ovarian cancers. The researchers conclusion was that above-normal weight was associated with almost 20% of all cancer deaths in the United States. “There’s an incredibly powerful link between obesity and cancer,” says oncologist Joyce Slingerland of the University of Miami, Florida. “Everyone’s heard of obesity’s effect on heart disease and diabetes, and we’re now beginning to understand that the cancer risk is just as great,” she says.
Although researchers and epidemiologists had long suspected that diet and cancer were linked, efforts to explain why being fat makes cancer more deadly have only begun to deliver results in the past decade.
So it is up to the people in society of that country they live in to take on responsible actions to make their country a better for all, not just one. I say that is becoming as healthy as possible that an individual can reach and without America has the answers in knowing how to make this happen 100% in our country.
A new study from American Cancer Society researchers finds it’s not just how much physical activity you get, but how much time you spend sitting that can affect your risk of death.
My final study supporting how obesity links with cancer:
Just think if this was you or someone you know in the world and this happens to you or them; GOD FORBID, but you can help yourself through prevention with losing the weight or just staying slim and tone if you already are. This will just decrease your risk of getting the cancer.
The JCCC study, led by Dr. Guido Eibl, JCCC member and professor-in-residence in the department of surgery at David Geffen School of Medicine, revealed that mice made obese with high-calorie, high-fat diets developed abnormally high numbers of these lesions.
This is the first study to show a direct causal link in an animal model between obesity and risk of this deadly pancreatic cancer. The JCCC study, led by Dr. Guido Eibl, JCCC member and professor-in-residence in the department of surgery at David Geffen School of Medicine, revealed that mice made obese with high-calorie, high-fat diets developed abnormally high numbers of these lesions. This is the first study to show a direct causal link in an animal model between obesity and risk of this deadly pancreatic cancer.
The mice eating the normal diet gained an average of approximately 7.2 g over 14 months. Mice on the high-fat, high-calorie diet more than doubled this with an average weight gain of 15.9 g.
Pathological tests showed that mice fed the normal diet had mostly normal pancreases with very few scattered PanIN lesions=intraepithelial neoplasias=precursors to pancreatic lesions. They are used as markers but can only be seen microscopically so a biopsy is needed. The mice fed high fat & cholesterol in their diet had significantly more PanIN lesions with less overall healthy pancreases.
The study showed that the mice fed a diet high in fats and calories gained significantly more weight, had abnormalities of their metabolism and increased insulin levels, and had marked pancreatic tissue inflammation with the development of PanIN lesions.
These observations suggest that such a diet like this which leads to weight gain, metabolism disturbances, pancreas inflammation and pancreas lesions that are precursors to cancer.
Obviously research is showing obesity has a link with cancer. We now know this information let’s make a move America and people elsewhere to become a healthier nation including world. For diversity is the US and other countries filled with all cultures, races and genders need to learn this knowledge to help make their country whether they were either born there and stayed or those born elsewhere moving to a new country, like America and we the people making up the country need to be responsible not just for yourselves but for your children and future generations in spreading good habits, good dieting, and good exercise to prevent high disease in the country for yourself and your children and the future generations by being a good role model in thinking=live healthy not unhealthy. In time this would play an impact on your countries economy and health care system in how its run.
References:
1 –American Institute for Cancer Research, Schernhammer ES et al. Circulating levels of insulin-like growth factors, their binding proteins, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005 Mar;14(3):699-704 ES et al. their binding proteins, and breast cancer risk—Cancer Epidemiol Biomarkers Prev. 2006 Mar;14(3):699-704/ AICR ScienceNow /Volume 16/Spring 2006
2 – Studies Help Clarify Link Between Obesity and Prostate Cancer Article date: March 2, 2006 Impact of Obesity on Prostate Cancer Recurrence After Radical Prostatectomy: Data from CaPSURE.” Published in the Nov., 2005 Urology (Vol. 66, No. 5: 1060-1065). First author: William W. Bassett, University of California, San Francisco.“Obesity, Serum Prostate Specific Antigen and Prostate Size: Implications for Prostate Cancer Detection.”Published in the Feb. 2006 Journal of Urology (Vol. 175, No. 2: 500-504). First author: Stephen J. Freedland, MD, Duke University School of Medicine.
3 –Director, Medical & Scientific Communications
American Cancer Society
david.sampson@cancer.org Article: “Body mass index and risk of ovarian cancer.” Michael F. Leitzmann, Corinna Koebnick, Kim N. Danforth, Louise A. Brinton, Steven C. Moore, Albert R. Hollenbeck, Arthur Schatzkin, and James V. Lacey, Jr. CANCER; Published Online: January 05, 2009 (DOI: 10.1002/cncr.24086); Print Issue Date: February 15, 2009.
4 –Medical News Today-“Direct Link to Obesity and Pancreatic Cancer” Author Belinda Weber
5 – Proceedings of the National Academy of Sciences of the United States of America –Article “Link between obesity and cancer” by Sarah C.P. Williams-Science Writer
6 – National Cancer Institute at the National Institute of health – Under their national cancer fact sheet regarding their article “Obesity and Cancer Risk”.