Cancercenter.org states the following:
”One of the most common risk factors for cancer is something we can’t do anything about—age. Our cancer risk increases as we get older, with the average age at diagnosis hovering around 68.
But a new study in Nature Reviews Clinical Oncology says that over the last few decades, doctors have been seeing dramatic increases in cancer in adults younger than 50. The disturbing trend has scientists searching for:
- Reasons behind the sharp increase in early-onset cancer
- How best to screen for or detect cancers in young adults
- Whether the cancers are different types of common cancers in older adults
- Which treatments show promise for younger people
Cancers in the under-50 age group may foreshadow an “emerging pandemic,” says the study’s researchers at Brigham and Women’s Hospital in Boston. Cancer patients under 50 are at a different point in their lives than the typical, older patient: They may be students, parents of young children, family breadwinners or caregivers to aging parents. Their cancer treatments may mean a different financial burden, one that hits during their prime income-earning years. They may also face higher risks of other health issues, including infertility, heart disease and secondary cancers.
“Young adults often have a more challenging landscape than older adults diagnosed with cancer,” says Toufic Kachaamy, MD, Interventional Program Specialist and Chief of Medicine at Cancer Treatment Centers of America® (CTCA), Phoenix (he was not involved in the study). “When you’re 40 and get cancer, there’s a good chance that you’ve never been sick before. One day, you’re out to dinner or a party, the next thing you know, you’re on chemotherapy.”
Which cancer types were studied?
Researchers looked at 14 cancers being diagnosed with increased frequency in adults who haven’t turned 50 yet:
- Breast cancer
- Colorectal cancer
- Endometrial cancer
- Esophageal cancer
- Extrahepatic bile duct cancer
- Gallbladder cancer
- Head and neck cancer
- Kidney cancer
- Liver cancer
- Multiple myeloma
- Pancreatic cancer
- Prostate cancer
- Stomach cancer
- Thyroid cancer
Colorectal cancer
Some of the highest increases in early-onset cancer are being seen in patients with colon cancer and rectal cancer. While colorectal incidence rates have dropped by almost 40 percent since 2000 among adults 50 and older, the rate is rising in those under 50. The latter trend may be linked to obesity levels that have exploded in the 18-25 age group, from 6.2 percent in 1976-80 to 32.7 percent in 2017-18.
Some researchers have thought that a higher body mass index (BMI)—or how much someone weighs compared to how tall he or she is—was a more significant risk factor for colon cancer than for rectal cancer. But that theory may not hold for early-onset cases, since researchers say rectal cancer is increasing in the United States at a faster rate than colon cancer.
Stomach cancer and esophageal cancer
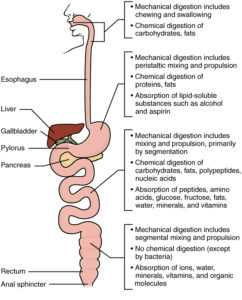
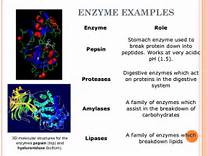
Stomach cancer and esophageal cancer, like colorectal cancers, are diseases of the gastrointestinal tract. Eight of the 14 early-onset cancers studied are cancers of the digestive system.
The findings suggest someone’s microbiome—the microorganisms floating around in the digestive tract—impacts cancer risk, either because of changes caused by poor nutrition, lifestyle factors such as smoking and drinking, or a significant increase in the use of antibiotics in recent decades.
Some risk factors for early-onset esophageal cancer include smoking, obesity and gastroesophageal reflux disease. Heavy alcohol consumption is considered a risk factor for all stomach cancers, including early-onset cases.
Breast cancer
The study, instead of using the under-50 and over-50 groupings typical for breast cancer analyses, looked at premenopausal and postmenopausal women. Breast cancer is rising in both groups, but at a faster rate among younger, premenopausal adults.
Some studies have shown that a large number of female breast cancer patients under 50 were not considered at high risk for the disease. Now, the American College of Radiology and the Society of Breast Imaging recommend women begin regular mammograms at age 40 instead of 50.
Some research on premenopausal breast cancer points to reproductive risk factors, obesity, physical inactivity, alcohol consumption and the prevalence of Western-style diets—ones high in red meats and processed foods—as contributors to early-onset breast cancer.
Lung cancer
Lung cancer was not included in the study because it’s been decreasing in both the under-50 and over-50 age groups. But the proportion of lung cancer cases among nonsmokers in the under-50 age group is rising.
Women also are making up an increasing proportion of lung cancers diagnosed in patients under 50, with men contributing to a steeper decline in those cases than women.
What caused cancer rates to rise in people under 50?
While increased screening may partially explain the rising number of early-onset diagnoses, researchers say that doesn’t tell the whole story.
“Evidence suggests that the earliest phase of carcinogenesis might start in early life or young adulthood, followed by intervals of up to several decades between initial cellular damage and clinical cancer detection,” the study’s authors wrote.
Since the mid-20th century, many unhealthy changes have affected diet, lifestyle, obesity, the environment and our microbiomes. Those changes may now be occurring earlier in life and may be making humans more susceptible to cancer at a younger age. Studies also suggest the increase in early-onset cancers may be part of the growing trend in chronic diseases affecting younger adults.
If you’re a parent or thinking about becoming one, your concern about early-onset cancer should extend to your children. The study says that a woman’s smoking, diet, alcohol consumption and obesity during pregnancy may play roles in her child’s future cancer risk. Providing your children with healthy meals, limiting processed and sugary foods in their diets, encouraging them to exercise, watching their weight and avoiding their exposure to second-hand smoke may help reduce their future cancer risk at a time when they’re too young to make good choices for themselves.
“We found that this risk is increasing with each generation,” says Shuji Ogino, MD, PhD, a professor and physician-scientist in the Department of Pathology at Brigham who was involved with the study. “For instance, people born in 1960 experienced higher cancer risk before they turn 50 than people born in 1950, and we predict that this risk level will continue to climb in successive generations.”
Which cancer risk factors affect young adults?
Some of the causes behind the increased cancer rates for adults under age 50 are thought to include:
- Drinking alcohol in excess
- Smoking tobacco
- Eating a Western diet
- Being obese or overweight
- Having type 2 diabetes
- Getting too little sleep, having abnormal sleep patterns and/or getting too little sleep during childhood
- Bearing children at a late age
- Having the first menstrual period at a young age
- Lower breast-feeding rates and increased formula consumption
- Using oral contraceptive
- Being exposed to environmental toxins
https://www.cancercenter.com/community/blog/2023/01/why-are-cancer-rates-rising-in-adults-under-50
Through Harvard.ed they state the following:
“In an extensive review, the team found that the early life “exposome,” which encompasses an individual’s diet, lifestyle, weight, environmental exposures, and microbiome, has changed substantially in the last several decades. They hypothesize that factors like the Western diet and lifestyle may be contributing to the rise in early onset cancer. The team acknowledged that this increased incidence of certain cancer types is, in part, due to early detection through cancer screening programs. They couldn’t precisely measure what proportion of this growing prevalence could solely be attributed to screening and early detection. However, they noted that increased incidence of many of the 14 cancer types is unlikely due to enhanced screening alone.
Possible risk factors for early onset cancer included alcohol consumption, sleep deprivation, smoking, obesity, and eating highly processed foods. Surprisingly, researchers found that while adult sleep duration hasn’t drastically changed over the several decades, children are getting far less sleep today than they were decades ago. Risk factors such as highly processed foods, sugary beverages, obesity, Type 2 diabetes, sedentary lifestyle, and alcohol consumption have all significantly increased since the 1950s.
“Among the 14 cancer types on the rise that we studied, eight were related to the digestive system. The food we eat feeds the microorganisms in our gut,” said Ugai. “Diet directly affects microbiome composition and eventually these changes can influence disease risk and outcomes.”
“https://news.harvard.edu/gazette/story/2022/09/researchers-report-dramatic-rise-in-early-onset-cancers/
Some of the causes behind the increased cancer rates for adults under age 50 are thought to include:
- Drinking alcohol in excess
- Smoking tobacco
- Eating a Western diet
- Being obese or overweight
- Having type 2 diabetes
- Getting too little sleep, having abnormal sleep patterns and/or getting too little sleep during childhood
- Bearing children at a late age
- Having the first menstrual period at a young age
- Lower breast-feeding rates and increased formula consumption
- Using oral contraceptive
- Being exposed to environmental toxins