Diabetes is still common in the United States. From 1980 through 2011, the number of Americans with diagnosed diabetes has more than tripled as of 2011 (from 5.6 million to 20.9 million).
30.3 million – The number of people in the U.S. who had diabetes in 2022. According to a the CDC’s most recent “National Diabetes Statistics Report” in 2023, an estimated 136 million adults in the United States are living with either diabetes or prediabetes.
Do you know how much it is costing in our country? Its a combination of factors that has caused such and increase in the disease of Diabetes in the U.S.
Factors:
-Look how much our population has increased with fast food companies pushing the unhealthy foods the sell in restaurants or food stores.
-Also people from other countries who permanently came into America becoming a citizen from 1980 to now and came in to the U.S. already eating poor OR picked up the bad habits of eating poor foods that the U.S. media pushes that is acceptable to enough by U.S. society (that just continues). This factor is adding to the diabetic population whether they came in the U.S. with it or got it when coming to live in America.
-Than people born in the U.S. with family having a history of diabetes or worse parents who did not watch good eating habits when raising their children who got obese putting them at high risk for diabetes.
–Ending line, these factors massively increased making the number of Diabetic Americans 3x higher since 1980.
-Than another factor is the illegals with diabetes also adds to the number of diabetic people in America; for they are not left out and are treated in hospitals with citizens of the U.S. If they come to an ER in the U.S. we treat them. Think of what the count is now with all these illegal people coming in the U.S. since the past 4 years with Former President Bidon and Harris in the office.
These factors all IMPACT an increase in the number of Diabetics in America!
Wake up America! We need to get this disease under better control! Diabetes increasing in the U.S. will not help disease overall in America!
Statistics:
That’s right. The metabolic condition is about as American as you can get, according to a the CDC’s most recent “National Diabetes Statistics Report” in 2023, an estimated 136 million adults in the United States are living with either diabetes or prediabetes, with the highest prevalence of diagnosed diabetes among American Indian/Alaskan Native adults, followed by non-Hispanic Black adults, Hispanic adults, non-Hispanic Asian adults, and then non-Hispanic White adults; the report also highlights disparities in diabetes prevalence based on socioeconomic factors like income and education level.
The report shows that nearly half of Americans have diabetes or prediabetes, which puts them at high risk for the condition. A good number of these folks haven’t been diagnosed and don’t even realize their predicament.
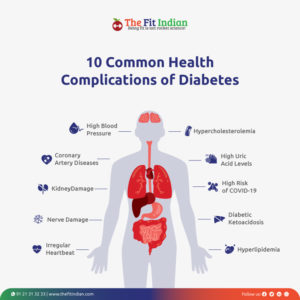
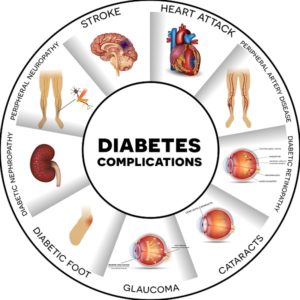
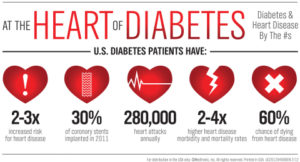
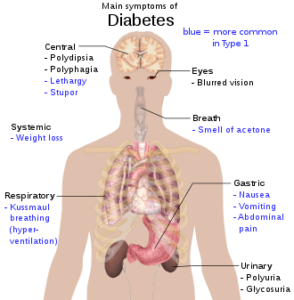
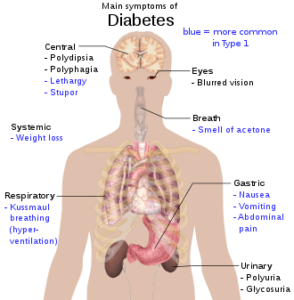
People with diabetes have too much sugar in their blood. If the disease isn’t controlled, they can wind up with heart disease, nerve damage, kidney problems, eye damage and other serious health problems.
That’s right. The metabolic condition is about as American as you can get, according to national report card on diabetes by the Centers for Disease Control and Prevention.
There are 2 types of Diabetes:
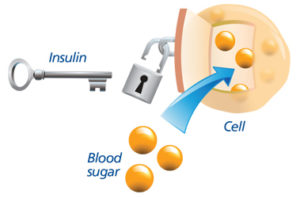
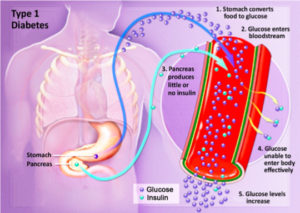
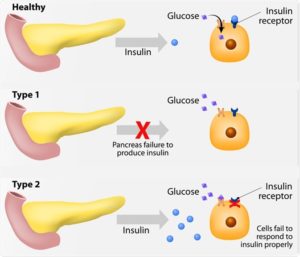
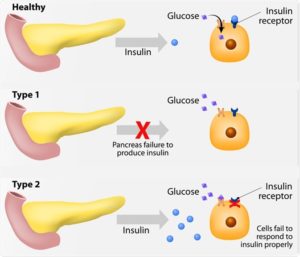
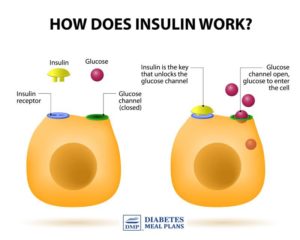
Type 1 diabetes was previously called insulin-dependent mellitus (IDDM) or juvenile-onset diabetes. This type of diabetes happens when the immune system ends up destroying beta cells in the body that come from our pancreas and they are the only cells in the human body that make the hormone INSULIN the regulates your glucose. Insulin allows glucose to transfer into the cells and tissues of our body to give them their energy to do their job in the body and nutrition to work properly=sugar-glucose. To live with this diabetes the person must have their insulin delivered by injection or a pump. This form of diabetes usually occurs in children or young adults but can occur at any age.
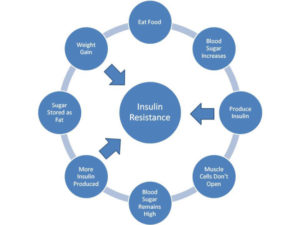
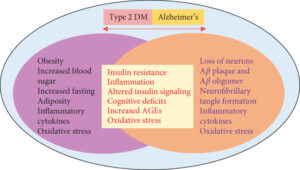
Type 2 diabetes was called non-insulin dependent diabetes mellitus (NIDDM) or adult-onset diabetes. In adults, type 2 diabetes accounts for about 90-95% of all diagnosed cases of diabetes. It usually begins as insulin resistance, a disease in which the cells do not use insulin properly due to the pancreas not making enough or the pancreas not secreting the correct form o of insulin to do its function. Ending line the insulin isn’t working properly. As the need for insulin rises, the pancreas gradually loses its ability to produce it.
Type 2 diabetes is associated with older age, OBESITY, family history of diabetes, history of gestational diabetes, impaired glucose metabolism, physical inactivity and race/ethnicity.
Gestational diabetes is a form of glucose intolerance diagnosed during pregnancy. Gestational diabetes occurs more frequently among African Americans, Hispanic/Latino Americans, and American Indians. It is also more common among obese women and women with a family history of diabetes. During pregnancy, gestational diabetes requires treatment to optimize maternal blood glucose levels to lessen the risk of complications in the infant.
Other types of diabetes result from; specific genetic conditions (such as maturity-onset diabetes of youth), surgery, medications, infections, pancreatic disease, and other illnesses. Such types of diabetes account for 1% to 5% of all diagnosed cases.
Treatment for Diabetes:
Diet, insulin, and oral medication to lower blood glucose levels are the foundation of diabetes treatment and management. Patient education and self-care practices are also important aspects of disease management that help people with diabetes lead normal lives or as normal as possible.
To survive, people with type 1 diabetes must have insulin delivered by injection or a pump.
Many people with type 2 diabetes can control their blood glucose by following a healthy meal plan and exercise program, losing excess weight, and taking oral medication.
Medications for each individual with diabetes will often change during the course of the disease. Some people with type 2 diabetes may also need insulin to control their blood glucose.
Self-management education or training is a key step in improving health outcomes and quality of life. It focuses on self-care behaviors, such as healthy eating, being active, and monitoring blood sugar.
The medications used for diabetes would be that your endocrinologist doctor would decide:
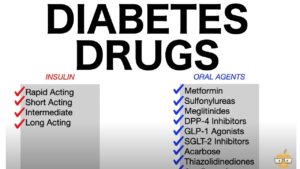

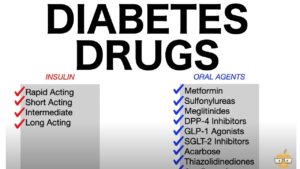
-Insulins-commonly in Type I DM but can be used if needed in Type II DM which the MD decides:
If you have type 1 diabetes, your body can’t make its own insulin. The goal of treatment is to replace the insulin that your pancreas can’t make.
Insulin is the most common type of medication used in type 1 diabetes treatment. There are more than 20 types sold in the United States.
It’s given as an infusion under the skin (with the help of an insulin pump) or as an injection.
There are multiple types of insulin. They vary based on how quickly they start working, how long they work, and whether they have a peak level of action.
The type of insulin you need depends on your body’s sensitivity to insulin and the severity of your insulin deficiency.
There are short acting, rapid acting, intermediate acting long acting, and combination insulins.
Also there is amylinomimetic. It’s an injectable medication that’s used before meals. It works by delaying the time your stomach takes to empty itself. It also reduces the secretion of the hormone glucagon after meals. These actions lower your blood sugar. Specifics are another topic in itself.
-Oral medications commonly used in type II diabetics; again specifics are another topic in itself.

If not doing treatment the diabetic will end up with severe complications to possibly death sooner in life than a compliant diabetic.
Pretty simple isn’t it but you have to the make a move quick if you haven’t yet! Take action and make changes if you need to!
How the cost of diabetes impacts America:
Diabetes is not only common and serious; it is also VERY COSTLY! This impacts medical insurance being so high since our population is so high in America. Let us take a look how:
The cost of treating diabetes is staggering. According to the American Diabetes Association, the annual cost of diabetes in medical expenses and lost productivity rose for $98 billion in 1997 to $132 billion in $2002 to $174 billion in 2007.
Two years ago in this post it stated one out of every 5 U.S. federal health care dollars is spent treating people with diabetes. The average yearly health care costs for a person without diabetes is 2,560 dollars; for a person with diabetes that figure soars to $11,744. Much of the human and financial costs can be avoided with proven diabetes prevention and management steps.
Now in 2022 the American Diabetes Association states “People with diagnosed diabetes incur average medical expenditures of $16,752 per year, of which about $9,601 is attributed to diabetes. On average, people with diagnosed diabetes have medical expenditures approximately 2.3 times higher than what expenditures would be in the absence of diabetes.” https://diabetes.org/about-us/statistics/cost-diabetes
Diabetes.org states now that “The estimated total economic cost of diagnosed diabetes in 2017 is $327 billion, a 26% increase from our previous estimate of $245 billion (in 2012 dollars).
The CDC states the following:
“The High Cost of Diabetes
Diabetes is the most expensive chronic condition in our nation.
- $1 out of every $4 in US health care costs is spent on caring for people with diabetes.
- $237 billionis spent each year on direct medical costs and another $90 billion on reduced productivity.
- The total economic cost of diabetes rose 60% from 2007 to 2017.
- 61% of diabetes costs are for people 65 years or older, which is mainly paid by Medicare.
- 48% to 64% of lifetime medical costs for a person with diabetes are for complications related to diabetes, such as heart disease and stroke.
So think if we decreased diabetes and many other diseases diabetes can cause how much we in America would decrease medical costs in America and help our economy drastically!!
If you agree be healthy and than those with diabetes (DM) being compliant will help you as an individual but compliant diabetics in numerous quantity will also help the economy. Even helping economy, more would be people without DM preventing DM from ever occuring. Both compliant diabetics and people living a healthy to prevent diabetes would drastically help our economy with decreasing the medical costs for diabetes.



 =
=