Possible causes of Epilepsy:
Their epilepsy that is diagnosed with a IDIOPATHIC cause – meaning unknown cause and the patient could grow out of it in childhood in some cases (not all) depending on the type of seizure disorder and if the child doesn’t grow out of it the condition becomes chronic (for life).
Genetic influence (heredity). Some types of epilepsy run in families. In these instances, it’s likely that there’s a genetic influence. Researchers have linked some types of epilepsy to specific genes. But some people have genetic epilepsy that isn’t hereditary. Genetic changes can occur in a child without being passed down from a parent.For most people, genes are only part of the cause of epilepsy. Certain genes may make a person more sensitive to environmental conditions that trigger seizures.
- A genetic tendency, passed down from one or both parents (inherited).
- A genetic tendency that is not inherited, but is a new change in the person’s genes.
Although heredity has been known since antiquity to cause epilepsy, the progress to date in identifying the genetic basis of epilepsy has been limited primarily to the discovery of single gene mutations that cause epilepsy in relatively rare families. For the more common types of epilepsy, heredity plays a subtler role, and it is thought that a combination of mutations in multiple genes likely determine an individual’s susceptibility to seizures, as well as the responsiveness to antiepileptic medications.
Epilepsy can be caused by genetic factors (inherited) or acquired (a etiology—cause) , although in most cases it arises in part from both. The neurology and neurological sciences of Stanford Epilepsy Center Dr. Robert S. Fischer Ph D. presents in the article Genetic Causes of Epilepsy.
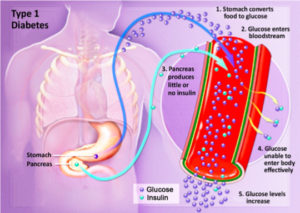
He also presents in this article our genes are the instruction set for building the human body. Genes reside on chromosomes.
Going to the basics is every person has 46 chromosomes, carrying a total of about 30,000 genes. We get half our chromosomes from our mother and half from our father. While genes determine the structure of our body, they also control the excitability of our brain cells. Defective genes can make hyperexcitable brain cells, which are prone to seizures.
In recent years, several epilepsy conditions have been linked to mutations in genes, but the matter is complicated by the fact that different genes may be involved in different circumstances.
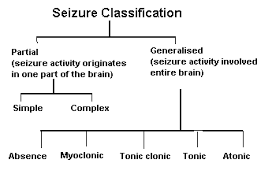
In general, the most common epilepsy conditions, including partial seizures, seem to be more acquired than genetic.
Gene testing will soon be able to identify predispositions to epilepsy, allowing doctors to help a patient get treatment and to assist with family counseling. One day, doctors may simply be able to swap a patient’s cheek, test his or her genes, and predict response to various epilepsy medicines, eliminating much of the trial and error in medication choice that goes on today. Eventually, we may even be able to repair or replace defective genes that predispose a person to epilepsy, a process called gene therapy.
Lastly, Dr. Robert Fischer Ph D presented in his article, that I found very interesting, the general population has about a 1% risk of developing epilepsy. Meanwhile, children of mothers with epilepsy have a 3 to 9% risk of inheriting this disease, while children of fathers have a 1.5 to 3% risk of inheritence. Still, the actual risk is upon the specific type of epilepsy. For example, partial seizures are less likely to run in families than are generalized seizures. In any event, with the usual forms of epilepsy, even if a parent does have the condition, there is more than a 90% chance that their child will not. So most epilepsies are acquired than inherited.
Clearly, genes determine a great deal of who we are, including our possible risk for epilepsy but slim versus a actual cause. But what happens to us in life and what we do is still the larger part of the risk for epilepsy.
A person given this diagnosis in the 1970’s, or before and even up to the early 1990’s was quiet about ever letting people know about this since in the 1970’s and back with lack of knowledge, information to the public and definitely technology versus now. Epilepsy is much more an accepted disease in the overall community compared to 20-25 years ago and back. Heck in the 1970’s and back these patients when having a seizure episode were characterized as “Freaks”. This was due to ignorance and lack of information to society/community but due to the past 20 to 25 years with the computer used more as a must in our lives with media, television and even our government they all have made it possible for society everywhere in the world to learn and understand diseases with acceptance in wanting to help those, particularly the US, but we still need a healthier America. It will take time to get there with the many multicultural lives that all live in the U.S. which practice differently on how important a healthy diet is with exercise balanced with rest. Also including stress well controlled is not always in America on their top priority list in living. Stress can even be a catalyst for a seizure but not the cause.
For a person diagnosed with or without a cause of epilepsy these steps in learning about the disease with higher technology and continuous research with medications over the years has allowed them to be able to live a completely healthy life doing the same things other people do without the disease but only if the patient is UNDER COMPLETE CONTROL which includes being COMPLIANT with your Rx; this does exist in America.
Compliant meaning taking their medications everyday as ordered by their neurologist with yearly or sooner follow-up visits with blood levels of the anti-seizure medications there on. This is the only way one with chronic epilepsy is guaranteed that living this way MAY stop the seizures from occurring (inactive epilepsy you can call it — meaning you’ll always have the disease but can put the seizure activity in a remission by medications preventing the seizure.)
Other Etiologies or Causes of Epilepsy:
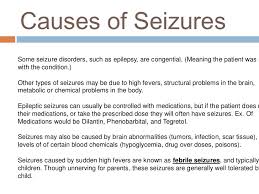
Epilepsy has no identifiable cause in about half the people with the condition. In the other half, the condition may be traced to various factors, including:
- Low oxygen during birth.
- Head trauma. Head trauma as a result of a car accident or other traumatic injury can cause epilepsy.
- Factors in the brain. Brain tumors can cause epilepsy. Epilepsy also may be caused by the way blood vessels form in the brain. People with blood vessel conditions such as arteriovenous malformations and cavernous malformations can have seizures. And in adults older than age 35, stroke is a leading cause of epilepsy.
- Infections. Meningitis, HIV, viral encephalitis and some parasitic infections can cause epilepsy.
- Injury before birth. Before they’re born, babies are sensitive to brain damage that could be caused by several factors. They might include an infection in the mother, poor nutrition or not enough oxygen. This brain damage can result in epilepsy or cerebral palsy.
Head trauma/Degenerative Disease like Alzheimer’s or Creutfeldz-Jacob or Huntington’s Chorea or Multiple Sclerosis or Pick’s Disease. There is also tumors or genetic disease or Stroke or Infections or Febrile seizures.
Different epilepsies are due to many different underlying causes. The causes can be complex, and sometimes hard to identify. A person might start having seizures because they have one or more of the following.
- A structural (sometimes called ‘symptomatic’) change in the brain, such as the brain not developing properly.
- A stroke or a tumour. A brain scan, such as Magnetic Resonance Imaging (MRI), may show this.
Some researchers now believe that the chance of developing epilepsy is probably always genetic to some extent, in that any person who starts having seizures has always had some level of genetic likelihood to do so. This level can range from high to low and anywhere in between.
Even if seizures start after a brain injury or other structural change, this may be due to both the structural change and the person’s genetic tendency to seizures, combined. This makes sense if we consider that many people might have a similar brain injury, but not all of them develop epilepsy afterwards.
Metabolic and Systemic Causes of Seizures:
a.) Electrolyte Imbalance=In the blood having acidosis, heavy metal poisoning, Hypocalcemia (low Ca+) , Hypocapnea (low carbon dioxide), Hypoglycemia (low glucose), Hypoxia (low oxygen), Sodium-Potassium imbalance, and than Systemic diseases (liver, renal failure, etc…). Then their is also toxemia of pregnancy, and water intoxication.
b.) Infections like meningitis, encephalitis, brain abcess. Structural changes due to genetic conditions such as tuberous sclerosis, or neurofibromatosis, which can cause growths affecting the brain.
Tuberous sclerosis – a genetic condition that causes growths in organs including the brain. Tuberous sclerosis can cause epilepsy.
Neurofibromatosis – a genetic condition that causes benign tumours to grow on the covering of nerves. Neurofibromatosis can cause epilepsy.
c.) Withdrawal of sedative-hypnotic drugs=Alcohol, Antiepileptic drugs, Barbiturates, Benzodiazepines.
d.) Iatrogenic drug overdose=Theopylline, Penicillin.
How Epilepsy is Diagnosed:
The purpose for intial visits is for the Neurologist to determine if the patient is having a seizure or something else and to determine what diagnotic tooling tests to start with to help the doctor to find out the problem. Apart from the description of the seizure, there are other things that can help to explain why your seizures have happened. Your medical history and any other medical conditions will also be considered as part of your diagnosis.
If you have a seizure you may not remember what has happened. It can be helpful to have a description of what happened from someone who saw your seizure, to pass on to your GP or specialist.
Here are some questions that may help you or someone who witnessed your seizure to record useful information about what happened:
Before the seizure
- Did anything trigger (set off) the seizure – for example, did you feel tired, hungry, or unwell?
- Did you have any warning that the seizure was going to happen?
- Did your mood change – for example, were you excited, anxious or quiet?
- Did you make any sound, such as crying out or mumbling?
- Did you notice any unusual sensations, such as an odd smell or taste, or a rising feeling in your stomach?
- Where were you and what were you doing before the seizure?
- TIME the seizure when it started and ended to tell the MD if not in the hospital!!
During the seizure
- Did you appear to be ‘blank’ or stare into space?
- Did you lose consciousness or become confused?
- Did you do anything unusual such as mumble, wander about or fiddle with your clothing?
- Did your colour change (become pale or flushed) and if so, where (face or lips)?
- Did your breathing change (for example, become noisy or look difficult)?
- Did any part of your body move, jerk or twitch?
- Did you fall down, or go stiff or floppy?
- Did you wet yourself?
- Did you bite your tongue or cheek?
After the seizure
- How did you feel after the seizure – did you feel tired, worn out or need to sleep?
- How long was it before you were able to carry on as normal?
- Did you notice anything else?
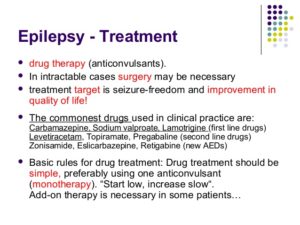
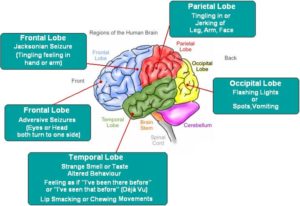
For F/U (follow up) visits is for the neurologist to see how well your seizures are under control by taking drug blood levels of the anti seizure medication your taking to make sure the medication is in a therapeutic drug level and if not he or she will make dose changes in the med(s) your on. Possible do a EEG (electroencephalogram); the only test to decipher if you have spikes in your brain waves indicating you had a seizure determining from which lobe of the brain is having the seizures (a 26 lead to wires on the brain, which is painless). Go to the expert for keeping you on the right track. Its just like based on the principle why a person gets a check up on there car by seeing the mechanic (the car’s doctor) who fixes it. The expert, the Neurologist, fix your seizures or get them under control.