Treatment Breakthroughs
In the early 1900s, there was no way to store blood. People with hemophilia who needed a transfusion typically received fresh whole blood from a family member. Life expectancy was 13 years old.
In 1901, the US Surgeon General’s Catalogue listed lime, inhaled oxygen and the use of thyroid gland or bone marrow, or hydrogen peroxide or gelatin, as treatments for hemophilia. By the 1930s, it was discovered that diluting certain snake venoms caused blood to clot. These treatment were used in patients with hemophilia.
By 1926, the US Surgeon General’s Catalogue contained an entire section on the use of blood transfusions to replace missing clotting factors. Physicians discovered that patients responded readily to infusions of plasma when given promptly after they sustained spontaneous joint and muscle bleeding.
In 1937 Harvard physicians Arthur Patek and FHL Taylor published a paper describing anti-hemophilia globulin found in plasma. It could decrease clotting time in patients with hemophilia.
By the late 1950s and early 1960s fresh frozen plasma was transfused in patients in the hospital. However, each bag of the plasma contained so little of the necessary clotting factor that huge volumes of it had to be administered. Many children experienced severe joint bleeds that were crippling. Intracranial hemorrhage could be fatal. By 1960, the life expectancy for a person with severe hemophilia was less than 20 years old.
A paper written by Robert Macfarlane, a British hematologist, in the journal Nature in 1964 described the clotting process in detail. The interaction of the different factors in blood clotting was termed the “coagulation cascade,” now called the clotting cascade.
In 1965, Dr. Judith Graham Pool, a researcher at Stanford University, published a paper on cryoprecipitate. In a major breakthrough, she discovered that the precipitate left from thawing plasma was rich in factor VIII. Because cryoprecipitate contained a substantial amount of factor in a smaller volume, it could be infused to control serious bleeding. Blood banks could produce and store the component, making emergency surgery and elective procedures for patients with hemophilia patients much more manageable.
By the 1970s, freeze-dried powdered concentrates containing factor VIII and IX became available. Factor concentrates revolutionized hemophilia care because they could be stored at home, allowing patients to “self-infuse” factor products, alleviating trips to the hospital for treatment.
By the mid-1980s, it was confirmed that HIV/AIDS could be transmitted through the use of blood and blood products, such as those used to treat hemophilia. Approximately half of the people with hemophilia in the US eventually became infected with HIV through contaminated blood products; thousands died. The overwhelming impact of HIV on the bleeding disorders community was felt into the next few decades.
The hepatitis C virus (HCV) infection was also transmitted through contaminated factor products, pooled from the blood of hundreds of thousands of donors. Before testing for HCV began in 1992, an estimated 44% of all people with hemophilia had contracted it. With the advent of more sophisticated screening methods and purification techniques, the risk of contracting HCV through factor products is virtually nil.
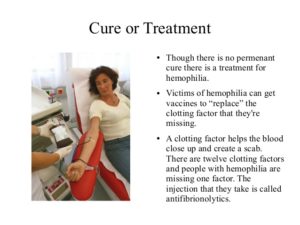
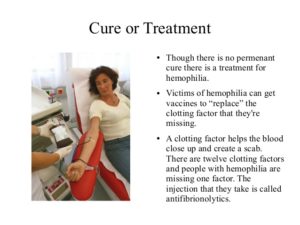
Treatment for hemophilia and other bleeding disorders advanced in the 1990s. Factor products became safer as tighter screening methods were implemented and advanced methods of viral inactivation were used. In addition, synthetic (not derived from plasma) factor products were manufactured using recombinant technologies. In 1992, the first recombinant factor VIII product was approved by the Food and Drug Administration (FDA). In 1997, the first recombinant factor IX product was granted FDA approval. Additional synthetic drugs, such as desmopressin acetate (DDAVP), were also introduced to treat mild-to-moderate hemophilia A and von Willebrand disease.
By 1995, prophylaxis, a preventive treatment regimen performed 2-3 times weekly in children with hemophilia, became more common. Since the advent of prophylaxis, most children in the developed world live with less pain, without the orthopedic damage associated with chronic bleeding. As a result, most children born with hemophilia in the US today can look forward to long, healthy and active lives.
However, some children develop inhibitors, or antibodies, to infused factor product. The development of a bypassing agent in 1997 offered these patients an alternative product to help stop bleeds and joint damage.
The early years of the 21st century have brought new recombinant products made without human or animal plasma derivatives, lowering the possibility risk for allergic reactions to the products or inhibitors? New longer-lasting products promise to decrease regular infusion rates from 2-3 times per week to once-weekly or even less.
In 2013, three separate gene therapy trials were begun at institutions across the country. They are testing the use of viruses as vector, or vehicles, to deliver factor IX genes into patients’ livers, correcting their hemophilia. Because the factor VIII gene is larger and more complicated to use, gene therapy clinical trials have not yet begun for patients with hemophilia A.
TIMELINE
1828 – Term “haemorrhaphilia” first used. Later shortened to “haemophilia.”
1926 – Erik von Willebrand identifies a bleeding disorder, later called von Willebrand disease (VWD)
1940s – whole blood transfusions given at hospital
1948 – National Hemophilia Foundation (NHF) opens as The Hemophilia Foundation, Inc.
1952 – Researchers describe what is now called factor IX clotting protein
1954 – NHF establishes a Medical Advisory Council, later called Medical and Scientific Advisory Council (MASAC)
1955 – First infusions of factor VIII in plasma form
1957 – Researchers in Sweden identify von Willebrand factor as the cause of VWD
1958 – First use of prophylaxis for hemophilia A
1964 – Dr. Judith Graham Pool discovers cryoprecipitate
1968 – First FVIII concentrate available
1970s – Primary prophylaxis therapy experiments begin
1970s – Freeze-dried plasma-derived factor concentrates available
1977 – Desmopressin identified to treat mild hemophilia and von Willebrand disease
1980s – Factor VIII, FIX and von Willebrand factor genes cloned
1982 – CDC reports first AIDS cases among people with hemophilia
1985 – First inactivated factor concentrates available
1992 – FDA approves first recombinant FVIII products
1995 – Prophylaxis becomes standard of treatment in US
1997 – FDA approves first recombinant FIX products
1998 – First human gene therapy trials begin
2000s – FDA approves first recombinant factor products made without human or animal plasma derivatives
2009 – FDA approves RiaSTAP to treat factor I deficiency
2011 – FDA approves Corifact to treat factor XIII deficiency
2013 – Gene therapy trials underway at three sites in the US
Check out a decade later 2023 treatments, tomorrow!