Men are more likely to experience hearing loss than women.
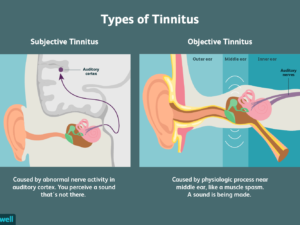
Of adults ages 65 and older in the United States, 12.3 percent of men and nearly 14 percent of women are affected by tinnitus. Tinnitus is identified more frequently in white individuals and the prevalence of tinnitus in almost twice as frequent in the South as in the Northeast.
Approximately 17 percent (36 million) of American adults report some degree of hearing loss.
There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing loss.
About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. Nine out of every 10 children who are born deaf are born to parents who can hear.
The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities.
Only 1 out of 5 people who could benefit from a hearing aid actually wears one.
Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old.
Roughly 25 million Americans have experienced tinnitus.
Approximately 188,000 people worldwide have received cochlear implants. In the United States, roughly 41,500 adults and 25,500 children have received them.
Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing loss affects only 1 ear in 9 out of 10 people who experience sudden deafness. Only 10 to 15 percent of patients with sudden deafness know what caused their loss.
Approximately 615,000 individuals have been diagnosed with Ménière’s disease in the United States. Another 45,500 are newly diagnosed each year.
Approximately 3 to 6 percent of all deaf children and perhaps another 3 to 6 percent of hard-of-hearing children have Usher syndrome. In developed countries such as the United States, about 4 babies in every 100,000 births have Usher syndrome.
One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma).
High levels of cotinine, the chemical that indicates exposure to tobacco smoke and second-hand smoke has been directly linked to higher risks of some types of hearing loss. **
More than 500 million people around the world are experiencing some form of hearing loss right now. Are you one of them?
Share :
If you have hearing loss, you are not alone. About one in six people experience some degree of hearing impairment over the course of their lives.
The effects may not be obvious…
Hearing loss affects people in different ways. Left undiagnosed or untreated, it can damage communications and erode relationships. Over time, hearing loss may degenerate from a strictly physical condition to a psychological one, which is just one of the reasons it is so important to seek a solution promptly. For most people with hearing loss, there is help. Properly fitted hearing aids improve communication for at least 90 percent of people with hearing loss.[1]
The cause of hearing loss may not be clear…
Hearing loss is not just the result of attending loud concerts or a factor of the aging process. Illness and infections can also play a part in damaging your hearing. A University of Wisconsin Medical School 2001 study[2] revealed that hearing loss occurred in nearly 80% of those who may have suffered from a heart attack. They further determined that individuals who exercised at least once a week experienced a 32 percent reduction in the risk of suffering from hearing loss compared to those who did not work out.
Other health issues associated with either temporary or permanent hearing loss include the following:
Sluggish or poor blood flow to the ear
High blood pressure
Sickle Cell Disease
Diabetes
Screenings for diabetes and other conditions typically do not include hearing tests. If you have one of these conditions, it’s probably a good idea to ask for a referral to a hearing care professional who can conduct a hearing screening to see if you are suffering from any kind of hearing loss.
Many other factors can lead to hearing loss, including your family history, repeated exposure to loud noises, injuries, and smoking.
Men are more likely to experience hearing loss than women.
Of adults ages 65 and older in the United States, 12.3 percent of men and nearly 14 percent of women are affected by tinnitus. Tinnitus is identified more frequently in white individuals and the prevalence of tinnitus is almost twice as frequent in the South as in the Northeast.
Approximately 17 percent (36 million) of American adults report some degree of hearing loss.
There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing loss.
About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. Nine out of every 10 children who are born deaf are born to parents who can hear.
The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities.
Only 1 out of 5 people who could benefit from a hearing aid actually wears one.
Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old.
Roughly 25 million Americans have experienced tinnitus.
Approximately 188,000 people worldwide have received cochlear implants. In the United States, roughly 41,500 adults and 25,500 children have received them.
Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing loss affects only 1 ear in 9 out of 10 people who experience sudden deafness. Only 10 to 15 percent of patients with sudden deafness know what caused their loss.
Approximately 615,000 individuals have been diagnosed with Ménière’s disease in the United States. Another 45,500 are newly diagnosed each year.
Approximately 3 to 6 percent of all deaf children and perhaps another 3 to 6 percent of hard-of-hearing children have Usher syndrome. In developed countries such as the United States, about 4 babies in every 100,000 births have Usher syndrome.
One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma).
High levels of cotinine, the chemical that indicates exposure to tobacco smoke and second-hand smoke has been directly linked to higher risks of some types of hearing loss. **
More than 500 million people around the world are experiencing some form of hearing loss right now. Are you one of them?
References:
1-World Health Organization. http://www.who.int/mediacentre/factsheets/fs300/en/
2-Torre P 3rd, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM. (2005). The association between cardiovascular disease and cochlear function in older adults. http://jslhr.asha.org/cgi/content/abstract/48/2/473
3-National Institute on Deafness and Other Communication Disorders (NIDCD).