
How is it transmitted?
Some viral hemorrhagic fevers are spread by mosquito or tick bites. Others are spread by contact with infected body fluids, such as blood, saliva or semen. A few varieties can be inhaled from infected rat feces or urine.
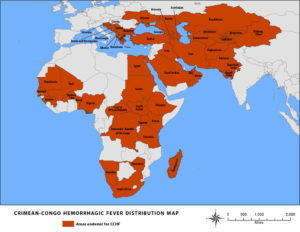
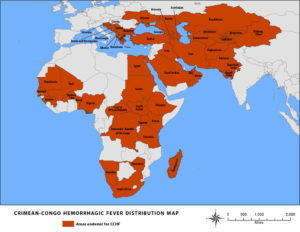
If you travel to an area where a particular hemorrhagic fever is common, you can be infected there but not develop symptoms until after you return home. Depending on the type of virus, it can take from two to 21 days for symptoms to develop.
Risk factors
Living in or traveling to an area where a particular viral hemorrhagic fever is common will increase your risk of becoming infected with that particular virus. Other factors that can increase your risk include:
- Working with infected people
- Slaughtering or eating infected animals
- Sharing needles to use intravenous drugs
- Having unprotected sex
- Working outdoors or in rat-infested buildings
- Being exposed to infected blood or other body fluids
Complications
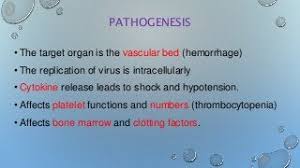
Viral hemorrhagic fevers can cause:
- Septic shock
- Multiorgan failure
- Death
Prevention
Preventing viral hemorrhagic fevers is challenging. If you live in, work in or travel to areas where these diseases are common, protect yourself from infection by using appropriate protective barriers when working with blood or body fluids. For example, wear gloves and eye and face shields. Precautions also include careful handling, disinfection and disposal of lab specimens and waste.
Get vaccinated
The yellow fever vaccine is generally considered safe and effective. However, in rare cases, serious side effects can occur. The yellow fever vaccine isn’t recommended for children younger than 9 months of age; pregnant women, especially during the first trimester; or people with compromised immune systems.
There’s also an Ebola vaccination that protects against one type of Ebola. Check with the Centers for Disease Control and Prevention about the status of the countries you’re visiting — some require certificates of vaccination for entry.
Avoid mosquitoes and ticks
Do your best to avoid these insects, especially when traveling in areas where there are outbreaks of viral hemorrhagic fevers. Wear light-colored long pants and long-sleeved shirts or, better yet, permethrin-coated clothing. Don’t apply permethrin directly to the skin.
Avoid being outside, if possible, at dusk and dawn when mosquitoes are most active, and apply mosquito repellent with a 20% to 25% concentration of DEET to your skin and clothing. If you’re staying in tented camps or in hotels, use bed nets and mosquito coils.
Guard against rodents
If you live where there are outbreaks of viral hemorrhagic fevers, take steps to keep rodents out of your home:
- Keep pet food covered and stored in rodent-proof containers.
- Store trash in rodent-proof containers, and clean the containers often.
- Dispose of garbage regularly.
- Make sure doors and windows have tightfitting screens.
- Keep woodpiles, stacks of bricks and other materials at least 100 feet from your house.
- Mow your grass closely and keep brush trimmed to within 100 feet of your house.