
How does colon-recto cancer even start:
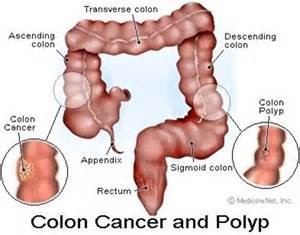
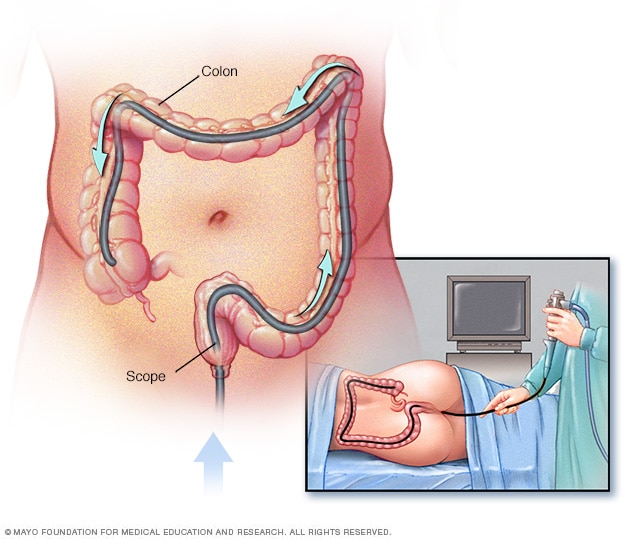
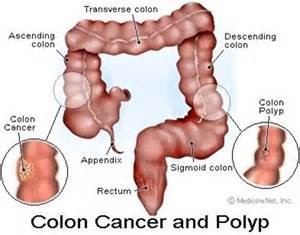
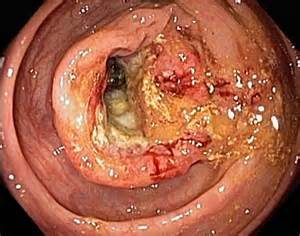
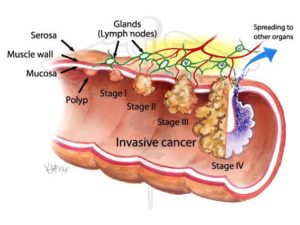
Most colorectal cancers start as a growth on the inner lining of the colon or rectum. These growths are called polyps.
Some types of polyps can change into cancer over time (usually many years), but not all polyps become cancer. The chance of a polyp turning into cancer depends on the type of polyp it is. There are different types of polyps.
- Adenomatous polyps (adenomas): These polyps sometimes change into cancer. Because of this, adenomas are called a pre-cancerous condition. The 3 types of adenomas are tubular, villous, and tubulovillous.
- Hyperplastic polyps and inflammatory polyps: These polyps are more common, but in general they are not pre-cancerous. Some people with large (more than 1cm) hyperplastic polyps might need colorectal cancer screening with colonoscopy more often.
- Sessile serrated polyps (SSP) and traditional serrated adenomas (TSA): These polyps are often treated like adenomas because they have a higher risk of colorectal cancer.
Other factors that can make a polyp more likely to contain cancer or increase someone’s risk of developing colorectal cancer include:
- If a polyp larger than 1 cm is found
- If more than 3 polyps are found
- If dysplasia is seen in the polyp after it’s removed. Dysplasia is another pre-cancerous condition. It means there’s an area in a polyp or in the lining of the colon or rectum where the cells look abnormal, but they haven’t become cancer.
The body is made up of trillions of living cells. Normal body cells grow, divide into new cells, and die in an orderly way. During the early years of a person’s life, while they are still growing, their normal cells divide faster. Once the person becomes an adult, most cells divide only to replace worn-out or dying cells or to repair injuries.
Cancer begins when cells in a part of the body start to grow out of control. There are many kinds of cancer, but they all start because of out-of-control growth of abnormal cells.
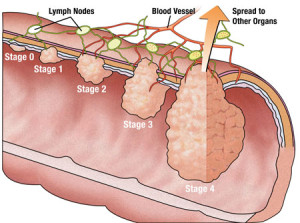
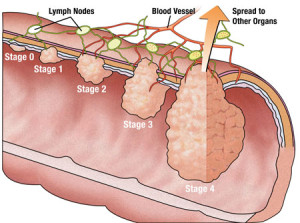
Cancer cell growth is different from normal cell growth. Instead of dying, cancer cells continue to grow and form new, abnormal cells. In most cases the cancer cells form a tumor. Cancer cells can also invade (grow into) other tissues, something that normal cells cannot do. Growing out of control and invading other tissues are what makes a cell a cancer cell.
Cells become cancer cells because of damage to DNA. DNA is in every cell and directs all its actions. In a normal cell, when DNA is damaged the cell either repairs the damage or the cell dies. In cancer cells, the damaged DNA is not repaired, but the cell doesn’t die like it should. Instead, this cell goes on making new cells that the body does not need. These new cells will all have the same damaged DNA as the first abnormal cell does.
People can inherit damaged DNA, but most often the DNA damage is caused by mistakes that happen while the normal cell is reproducing or by something in our environment. Sometimes the cause of the DNA damage is something obvious, like cigarette smoking. But often no clear cause is found.
Cancer cells often travel to other parts of the body, where they begin to grow and form new tumors that replace normal tissue. This process is called metastasis. It happens when the cancer cells get into the bloodstream or lymph vessels of our body.
No matter where a cancer may spread, it is always named for the place where it started. For example, breast cancer that has spread to the liver is still called breast cancer, not liver cancer
Different types of cancer can behave very differently. For example, lung cancer and breast cancer are very different diseases. They grow at different rates and respond to different treatments. This is why people with cancer need treatment that is aimed at their particular kind of cancer.
Not all tumors are cancerous. Tumors that aren’t cancer are called benign. Benign tumors can cause problems – they can grow very large and press on healthy organs and tissues. But they cannot grow into (invade) other tissues. Because they can’t invade, they also can’t spread to other parts of the body (metastasize). These tumors are rarely life threatening.
Their are risk factors in getting colon cancer as well as other cancer and noncancerous diseases BUT remember their are modifiable risk factors leading to disease which are factors we can’t control being 4 areas 1.)Race 2.)Age 3.) Sex 4.) Heredity in the family (particularly nuclear and grandparents meaning higher risk than a first cousin or second cousin and down the family tree).
Risk Factors to colon cancer can be:
Most colorectal cancers occur in people without a family history of colorectal cancer. Still, as many as 1 in 5 people who develop colorectal cancer have other family members who have been affected by this disease. People with a history of colorectal cancer in one or more first-degree relatives (parents, siblings, or children) are at increased risk. The risk is about doubled in those with only one affected first-degree relative=Nuclear Family. It is even higher if that relative was diagnosed with cancer when they were younger than 45, or if more than one first-degree relative is affected.
The reasons for the increased risk are not clear in all cases. Cancers can “run in the family” because of inherited genes, shared environmental factors, or some combination of these.
Having family members who have had adenomatous polyps is also linked to a higher risk of colon cancer. (Adenomatous polyps are the kind of polyps that can become cancerous.)
1-Inherited syndromes
About 5% to 10% of people who develop colorectal cancer have inherited gene defects (mutations) that can cause family cancer syndromes and lead to them getting the disease. These syndromes often lead to cancer that occurs at a younger age than is usual.
The most common inherited syndromes linked with colorectal cancers are familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (HNPCC), but other rarer syndromes can also increase colorectal cancer risk.
Familial adenomatous polyposis (FAP): FAP is caused by changes (mutations) in the APC gene that a person inherits from his or her parents. About 1% of all colorectal cancers are due to FAP.
The most common type of FAP causes people to develop hundreds or thousands of polyps in their colon and rectum, usually in their teens or early adulthood.
Hereditary non-polyposis colon cancer (HNPCC): HNPCC, also known as Lynch syndrome, accounts for about 2% to 4% of all colorectal cancers.
The cancers in this syndrome also develop when people are relatively young, although not as young as in FAP. People with HNPCC may also have polyps, but they only have a few, not hundreds as in FAP. The lifetime risk of colorectal cancer in people with this condition may be as high as 80%.
Turcot syndrome: This is a rare inherited condition in which people are at increased risk of adenomatous polyps and colorectal cancer, as well as brain tumors. There are actually 2 types of Turcot syndrome:
- One can be caused by gene changes similar to those seen in FAP, in which cases the brain tumors are medulloblastomas.
- The other can also be caused by gene changes similar to those seen in HNPCC, in which cases the brain tumors are glioblastomas.
- MUTYH-associated polyposis:Racial and ethnic background 1. Jews of Eastern European descent (Ashkenazi Jews) have one of the highest colorectal cancer risks of any ethnic group in the world. Several gene mutations leading to an increased risk of colorectal cancer have been found in this group. People with type 2 (usually non-insulin dependent) diabetes have an increased risk of developing colorectal cancer. Both type 2 diabetes and colorectal cancer share some of the same risk factors (such as excess weight). But even after taking these factors into account, people with type 2 diabetes still have an increased risk. They also tend to have a less favorable prognosis (outlook) after diagnosis.
2-Night shift workers are prone to cancers (colon/rectal and breast cancer).
3-Previous treatment for certain cancers –
Several studies have suggested that men who had radiation therapy to treat prostate cancer might have a higher risk of rectal cancer because the rectum receives some radiation during treatment. Men should consider the many possible side effects of prostate cancer treatment when making treatment decisions. Some doctors recommend that the risk of rectal cancer should be considered as one of those possible side effects but the patient is always responsible in doing research on their own before making the final decisions of treatment. They choose the treatment they feel is the best choice; not the doctor.
- Some studies have found that men who survive testicular cancer seem to have a higher rate of colorectal cancer and some other cancers. This might be because of the treatments they have received.
4-Factors less clear but can effect risk for colon cancer:
1-Type 2 diabetes
2-Racial Group African Americans have the highest colorectal cancer incidence and mortality rates of all racial groups in the United States. The reasons for this are not yet understood.
3-Peutz-Jeghers syndrome: People with this rare inherited condition tend to have freckles around the mout (and sometimes on the hands and feet) and a special type of polyp in their digestive tracts (called hamartoma). They are at greatly increased risk for colorectal cancer, as well as several other cancers, which usually appear at a younger than normal age. This syndrome is caused by mutations in the gene STK1. People with this syndrome develop colon polyps which will become cancerous if the colon is not removed.
Patients undergo lifelong surveillance of organs to monitor for cancer and prevent secondary problems from the polyps.
REVISED 3/05/2023


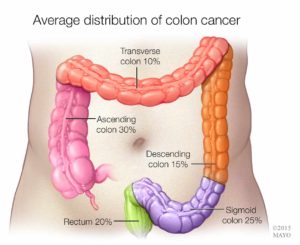
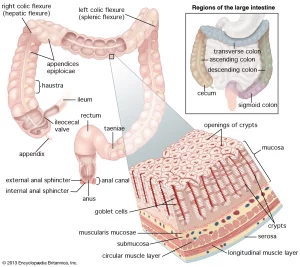
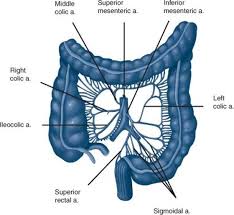
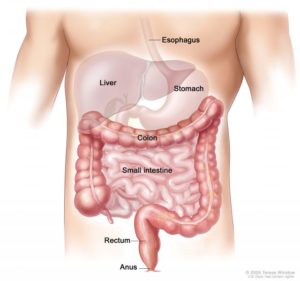
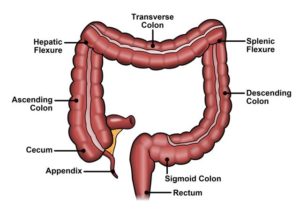 the colon to rectum
the colon to rectum