Blood cancer is a very broad term that describes multiple types of cancer. The common factor is that the cancer originates in blood cells and can spread throughout the body via the bloodstream or through the lymphatic system. White blood cells are the immune cells in our bodies that fight disease. Red blood cells carry oxygen throughout the body and remove carbon dioxide. Platelets are for clotting. Remember most importantly what was stated in Part I all cells are created by the bone marrow and then after created released out in the bloodstream (a free flowing unit system in the body that cells move along in going from tissues in the toes to the brain). When cancer cells created by marrow also go in the bloodstream allowing the cancer cells to free float through -out the bloodstream.
The different types of blood cancer are classified by the cell type that has become cancerous, where the cancer is located in the body, and how fast the cancer is progressing.
The three most common major types of blood cancer are myeloma, leukemia, lymphoma.
What is leukemia?
Leukemia usually involves the white blood cells. Your white blood cells are potent infection fighters — they normally grow and divide in an orderly way, as your body needs them. But in people with leukemia, the bone marrow produces abnormal white blood cells, which don’t function properly. There are many types of leukemia, which are classified by the specific type of white blood cell involved. White blood cells include the neutrophils and monocytes, which ingest (eat) bacteria and other germs; eosinophils and basophils, which are involved in allergic reactions; and lymphocytes, which play a key role in our body’s immune system.
Leukemia begins within the bone marrow, which is the soft spongy tissue inside our bones. In adults, remember we said yesterday bone marrow is found mainly in the flat bones, like the pelvis, skull, breastbone, ribs, shoulders, and vertebrae.
The bone marrow is where blood cells are made in a complex biological process called “hematopoiesis.” When a blood cell in the bone marrow changes to become cancerous, it can crowd out other cells and spread to the rest of the body via its primary channel the bloodstream.
What are the major types of leukemia?
There are four major sub-types of leukemia. Your specific diagnosis depends on how quickly the cancer grows and in which blood cell type it originates. Acute types of leukemia affect very young white blood cells and can progress rapidly. Chronic leukemias affect slightly more mature cells and progress more slowly. Lymphocytic leukemias affect white blood cells called lymphocytes, whereas myeloid leukemias affect cells that are destined to become any other type of blood cell.
- Acute lymphocytic leukemia (ALL)
- Chronic lymphocytic leukemia (CLL)
- Acute myeloid leukemia (AML)
- Chronic myeloid leukemia (CML)
What is lymphoma?
Lymphoma is a cancer that begins in the lymphatic system, which is part of the immune system. The lymphatic system is made up mainly of immune cells. We said yesterday they are called lymphocytes. B-cells and T-cells are the main lymphocytes, and each has a specific function in protecting our bodies from disease.
Lymphoma originates in lymph tissues, which can be found in many parts of the body, including in the lymph nodes, thymus, tonsils, adenoids, spleen, lymphatic vessels, and parts of the digestive system. If you have been diagnosed with lymphoma, your specific symptoms will depend on where your tumor began.
What are the major types of lymphoma?
There are two major sub-types of lymphoma. Your diagnosis depends on the type of cell where the cancer originated plus other characteristics of the tumor. Hodgkin lymphoma is characterized by the presence of Reed-Sternberg cells, which are named after the researchers who discovered them. Non-Hodgkin lymphoma does not have Reed-Sternberg cells.
- Hodgkin lymphoma
- Non-Hodgkin lymphoma
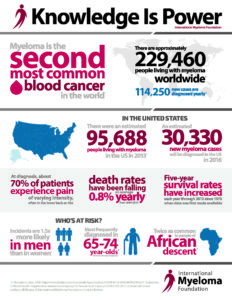
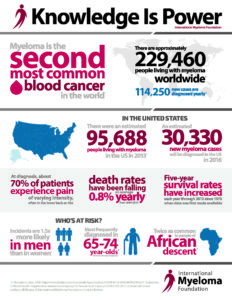
What is Multiple Myeloma?
Multiple myeloma is a cancer of plasma cells (B and T cells). Multiple myeloma is a cancer of plasma cells. Normal plasma cells are found in the bone marrow and are an important part of the immune system.The immune system is made up of several types of cells that work together to fight infections and other diseases.
We stated yesterday myeloma is most often found in bone marrow. Remember normal plasma cells are found in the bone marrow & an important part of the immune system.
The immune system is made up of several types of cells that work together to fight infections and other diseases. Lymphocytes (lymph cells) are one of the main types of white blood cells in the immune system and include T cells and B cells. Lymphocytes are in many areas of the body, such as lymph nodes, the bone marrow, the intestines, and the bloodstream.
When B cells respond to an infection, they mature and change into plasma cells. Plasma cells make the antibodies (also called immunoglobulins) that help the body attack and kill germs.
When plasma cells become cancerous=cancer cells (intially made in the bone marrow than released in the blood), they multiply and begin to crowd out healthy cells and produce abnormal antibodies called M proteins. This continues to to replicate till the body dies or some treatment takes over decreasing them by destroying them (Ex. Chemo) or possibly putting the patient in remission.
What are the major types of myeloma?
There are four major sub-types of myeloma. Diagnosis depends on how localized or spread out the cancer has become and where it originated. The most common form of myeloma is multiple myeloma. Over 90% of people with myeloma have multiple myeloma.
- Multiple myeloma -This is the one we will be discussing in this topic.
- Plasmacytoma
- Localized myeloma
- Extramedullary myelom
Multiple Myeloma Complications:
In multiple myeloma, the overgrowth of plasma cells in the bone marrow can crowd out normal blood-forming cells:
1-Leading to low cell counts=RBCs-low in iron/anemia, level of platelets in the become low (called thrombocytopenia)=increased bleeding and bruising & WBCs low called leukopenia=problems fighting infections.
2-Myeloma cells make a substance that tells the osteoclasts to speed up dissolving the bone. So old bone is broken down without new bone to replace it, making the bones painful, weak, thinning the bones and easy to break.
3-Abnormal plasma cells cannot protect the body from infections. As mentioned before, normal plasma cells produce antibodies that attack germs. In multiple myeloma, the myeloma cells crowd out the normal plasma cells, so that antibodies to fight the infection can’t be made. The antibody made by the myeloma cells does not help fight infections. That’s because the myeloma cells are just many copies of the same plasma cell – all making copies of the same exact (or monoclonal) antibody.
A monoclonal gammopathy is when plasma cells make too many copies of the same antibody. It is usually found on a routine blood test when looking for other conditions.In monoclonal gammopathy of undetermined significance (MGUS), abnormal plasma cells make many copies of the same antibody (called a monoclonal protein). However, these plasma cells do not form an actual tumor or mass and do not cause any of the problems seen in multiple myeloma. MGUS usually does not affect a person’s health. It doesn’t cause weak bones, high calcium levels, kidney problems, or low blood counts.
4-Myeloma cells make an antibody that can harm the kidneys, leading to kidney damage and even kidney failure.
Factors that may increase your risk of multiple myeloma include:
- Increasing age. Your risk of multiple myeloma increases as you age, with most people diagnosed in their mid-60s.
- Male sex. Men are more likely to develop the disease than are women.
- Black race. Black people are about twice as likely to develop multiple myeloma as are white people.
- Family history of multiple myeloma. If a brother, sister or parent has multiple myeloma, you have an increased risk of the disease.
- Personal history of a monoclonal gammopathy of undetermined significance (MGUS). Every year 1 percent of the people with MGUS in the United States develop multiple myeloma.
Diagnosing Multiple Myeloma:
- Blood tests. Laboratory analysis of your blood may reveal the M proteins produced by myeloma cells. Another abnormal protein produced by myeloma cells — called beta-2-microglobulin — may be detected in your blood and give your doctor clues about the aggressiveness of your myeloma.Additionally, blood tests to examine your kidney function, blood cell counts, calcium levels and uric acid levels can give your doctor clues about your diagnosis.
- Urine tests. Analysis of your urine may show M proteins, which are referred to as Bence Jones proteins when they’re detected in urine.
- Examination of your bone marrow. Your doctor may remove a sample of bone marrow for laboratory testing. The sample is collected with a long needle inserted into a bone (bone marrow aspiration and biopsy).In the lab, the sample is examined for myeloma cells. Specialized tests, such as fluorescence in situ hybridization (FISH) can analyze myeloma cells to understand their genetic abnormalities. Tests are also done to measure the rate at which the myeloma cells are dividing.
- Imaging tests. Imaging tests may be recommended to detect bone problems associated with multiple myeloma. Tests may include an X-ray, MRI, CT or positron emission tomography (PET).
After someone is diagnosed with cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging (I,II,III,IV). The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it.
Treatment:
1-Targeted therapy. Targeted drug treatment focuses on specific abnormalities within cancer cells that allow them to survive. Bortezomib (Velcade), carfilzomib (Kyprolis) and ixazomib (Ninlaro) are targeted drugs that block the action of a substance in myeloma cells that breaks down proteins. This action causes myeloma cells to die. Targeted-therapy drugs may be administered through a vein in your arm or in pill form.
Other targeted-therapy treatments include monoclonal antibody drugs that bind to the specific proteins present on myeloma cells, causing them to die.
2-Biological therapy. Biological therapy drugs use your body’s immune system to fight myeloma cells. The drugs thalidomide (Thalomid), lenalidomide (Revlimid) and pomalidomide (Pomalyst) enhance the immune system cells that identify and attack cancer cells. These medications are commonly taken in pill form.
3-Chemotherapy. Chemotherapy drugs kill fast-growing cells, including myeloma cells. Chemotherapy drugs can be given through a vein in your arm or taken in pill form. High doses of chemotherapy drugs are used before a bone marrow transplant.
4-Corticosteroids. Corticosteroids, such as prednisone and dexamethasone, regulate the immune system to control inflammation in the body. They are also active against myeloma cells. Corticosteroids can be taken in pill form or administered through a vein in your arm.
5-Bone marrow transplant. A bone marrow transplant, also known as a stem cell transplant, is a procedure to replace your diseased bone marrow with healthy bone marrow.
Before a bone marrow transplant, blood-forming stem cells are collected from your blood. You then receive high doses of chemotherapy to destroy your diseased bone marrow. Then your stem cells are infused into your body, where they travel to your bones and begin rebuilding your bone marrow.
6-Radiation therapy. This treatment uses beams of energy, such as X-rays and protons, to damage myeloma cells and stop their growth. Radiation therapy may be used to quickly shrink myeloma cells in a specific area — for instance, when a collection of abnormal plasma cells form a tumor (plasmacytoma) that’s causing pain or destroying a bone.