Archive | November 2023
QUOTE FOR FRIDAY:
“Cancer is the name given to a collection of related diseases. In all types of cancer, some of the body’s cells begin to divide without stopping and spread into surrounding tissues.
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and divide to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
When cancer develops, however, this orderly process breaks down. As cells become more and more abnormal, old or damaged cells survive when they should die, and new cells form when they are not needed. These extra cells can divide without stopping and may form growths called tumors.
Many cancers form solid tumors, which are masses of tissue. Cancers of the blood, such as leukemias, generally do not form solid tumors.
Cancerous tumors are malignant, which means they can spread into, or invade, nearby tissues. In addition, as these tumors grow, some cancer cells can break off and travel to distant places in the body through the blood or the lymph system and form new tumors far from the original tumor.
Unlike malignant tumors, benign tumors do not spread into, or invade, nearby tissues.
Cancer cells differ from normal cells in many ways that allow them to grow out of control and become invasive. One important difference is that cancer cells are less specialized than normal cells. That is, whereas normal cells mature into very distinct cell types with specific functions, cancer cells do not. This is one reason that, unlike normal cells, cancer cells continue to divide without stopping.
In addition, cancer cells are able to ignore signals that normally tell cells to stop dividing or that begin a process known as programmed cell death, or apoptosis, which the body uses to get rid of unneeded cells.
Cancer cells may be able to influence the normal cells, molecules, and blood vessels that surround and feed a tumor—an area known as the microenvironment. For instance, cancer cells can induce nearby normal cells to form blood vessels that supply tumors with oxygen and nutrients, which they need to grow. These blood vessels also remove waste products from tumors.
Cancer can be inherited and not.
The genetic changes that contribute to cancer tend to affect three main types of genes—proto-oncogenes, tumor suppressor genes, and DNA repair genes. These changes are sometimes called “drivers” of cancer.
The genetic changes that contribute to cancer tend to affect three main types of genes—proto-oncogenes, tumor suppressor genes, and DNA repair genes. These changes are sometimes called “drivers” of cancer.”
Georgetown Lombardi Comprehensive Cancer Center (https://ruesch.georgetown.edu/whatiscancer/)
Know Cancer-Normal vs. Cancer Cells, how cancer arises, drivers of cancer, when cancer spreads and tissue changes are not cancerous!
Cancer is the uncontrolled growth of abnormal cells in the body. Cancer develops when the body’s normal control mechanism stops working. Old cells do not die and instead grow out of control, forming new, abnormal cells. These extra cells may form a mass of tissue, called a tumor. Some cancers, such as leukemia, do not form tumors.
Cancer may occur anywhere in the body. In women, breast cancer is one of the most common. In men, it’s prostate cancer. Lung cancer and colorectal cancer affect both men and women in high numbers.
There are five main categories of cancer:
- Carcinomas begin in the skin or tissues that line the internal organs.
- Sarcomas develop in the bone, cartilage, fat, muscle or other connective tissues.
- Leukemia begins in the blood and bone marrow.
- Lymphomas start in the immune system.
- Central nervous system cancers develop in the brain and spinal cord
Differences between Cancer Cells and Normal Cells
Cancer cells differ from normal cells in many ways that allow them to grow out of control and become invasive. One important difference is that cancer cells are less specialized than normal cells. That is, whereas normal cells mature into very distinct cell types with specific functions, cancer cells do not. This is one reason that, unlike normal cells, cancer cells continue to divide without stopping.
In addition, cancer cells are able to ignore signals that normally tell cells to stop dividing or that begin a process known as programmed cell death, or apoptosis, which the body uses to get rid of unneeded cells.
Cancer cells may be able to influence the normal cells, molecules, and blood vessels that surround and feed a tumor—an area known as the micro-environment. For instance, cancer cells can induce nearby normal cells to form blood vessels that supply tumors with oxygen and nutrients, which they need to grow. These blood vessels also remove waste products from tumors.
Cancer cells are also often able to evade the immune system, a network of organs, tissues, and specialized cells that protects the body from infections and other conditions. Although the immune system normally removes damaged or abnormal cells from the body, some cancer cells are able to “hide” from the immune system.
Tumors can also use the immune system to stay alive and grow. For example, with the help of certain immune system cells that normally prevent a runaway immune response, cancer cells can actually keep the immune system from killing cancer cells.
How Cancer Arises
Cancer is a genetic disease—that is, it is caused by changes to genes that control the way our cells function, especially how they grow and divide.
Genetic changes that cause cancer can be inherited from our parents. They can also arise during a person’s lifetime as a result of errors that occur as cells divide or because of damage to DNA caused by certain environmental exposures. Cancer-causing environmental exposures include substances, such as the chemicals in tobacco smoke, and radiation, such as ultraviolet rays from the sun. (Our Cancer Causes and Prevention section has more information.)
Each person’s cancer has a unique combination of genetic changes. As the cancer continues to grow, additional changes will occur. Even within the same tumor, different cells may have different genetic changes.
In general, cancer cells have more genetic changes, such as mutations in DNA, than normal cells. Some of these changes may have nothing to do with the cancer; they may be the result of the cancer, rather than its cause.
“Drivers” of Cancer
The genetic changes that contribute to cancer tend to affect three main types of genes—proto-oncogenes, tumor suppressor genes, and DNA repair genes. These changes are sometimes called “drivers” of cancer.
Proto-oncogenes are involved in normal cell growth and division. However, when these genes are altered in certain ways or are more active than normal, they may become cancer-causing genes (or oncogenes), allowing cells to grow and survive when they should not.
Tumor suppressor genes are also involved in controlling cell growth and division. Cells with certain alterations in tumor suppressor genes may divide in an uncontrolled manner.
DNA repair genes are involved in fixing damaged DNA. Cells with mutations in these genes tend to develop additional mutations in other genes. Together, these mutations may cause the cells to become cancerous.
As scientists have learned more about the molecular changes that lead to cancer, they have found that certain mutations commonly occur in many types of cancer. Because of this, cancers are sometimes characterized by the types of genetic alterations that are believed to be driving them, not just by where they develop in the body and how the cancer cells look under the microscope.
When Cancer Spreads
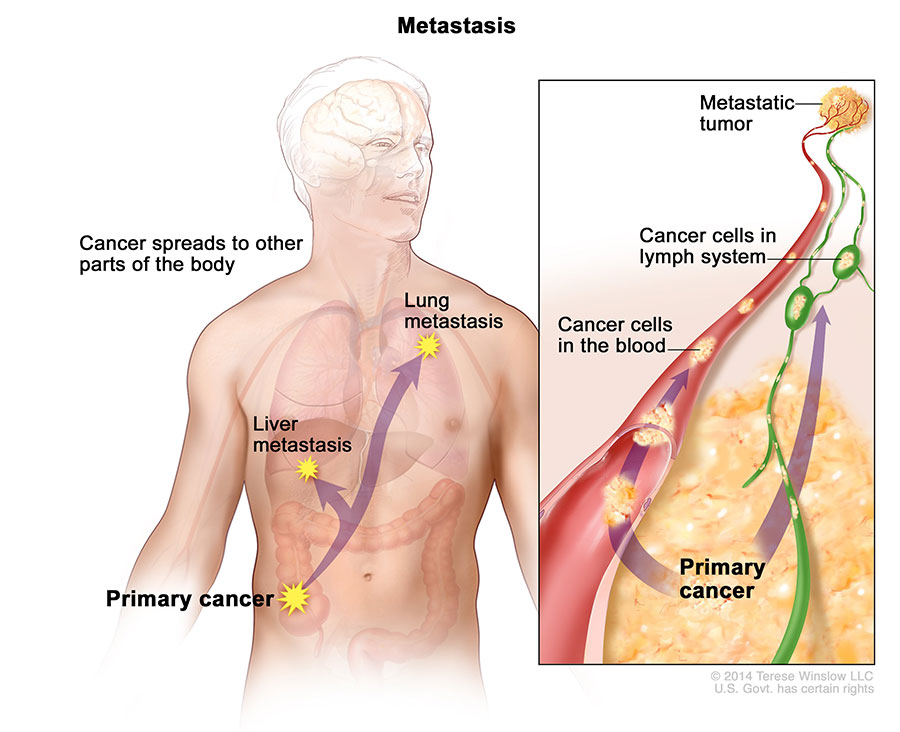
In metastasis, cancer cells break away from where they first formed (primary cancer), travel through the blood or lymph system, and form new tumors (metastatic tumors) in other parts of the body. The metastatic tumor is the same type of cancer as the primary tumor.
A cancer that has spread from the place where it first started to another place in the body is called metastatic cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
Metastatic cancer has the same name and the same type of cancer cells as the original, or primary, cancer. For example, breast cancer that spreads to and forms a metastatic tumor in the lung is metastatic breast cancer, not lung cancer.
Under a microscope, metastatic cancer cells generally look the same as cells of the original cancer. Moreover, metastatic cancer cells and cells of the original cancer usually have some molecular features in common, such as the presence of specific chromosome changes.
Treatment may help prolong the lives of some people with metastatic cancer. In general, though, the primary goal of treatments for metastatic cancer is to control the growth of the cancer or to relieve symptoms caused by it. Metastatic tumors can cause severe damage to how the body functions, and most people who die of cancer die of metastatic disease.
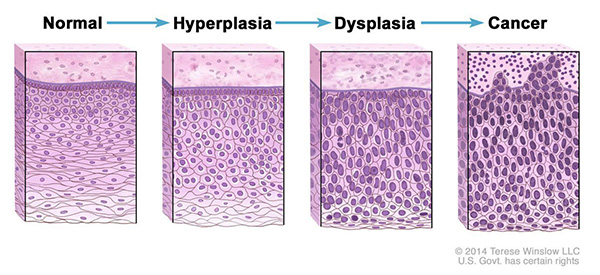
Tissue Changes that Are Not Cancer
Not every change in the body’s tissues is cancer. Some tissue changes may develop into cancer if they are not treated, however. Here are some examples of tissue changes that are not cancer but, in some cases, are monitored:
Hyperplasia occurs when cells within a tissue divide faster than normal and extra cells build up, or proliferate. However, the cells and the way the tissue is organized look normal under a microscope. Hyperplasia can be caused by several factors or conditions, including chronic irritation.
Dysplasia is a more serious condition than hyperplasia. In dysplasia, there is also a buildup of extra cells. But the cells look abnormal and there are changes in how the tissue is organized. In general, the more abnormal the cells and tissue look, the greater the chance that cancer will form.
Some types of dysplasia may need to be monitored or treated. An example of dysplasia is an abnormal mole (called a dysplastic nevus) that forms on the skin. A dysplastic nevus can turn into melanoma, although most do not.
An even more serious condition is carcinoma in situ. Although it is sometimes called cancer, carcinoma in situ is not cancer because the abnormal cells do not spread beyond the original tissue. That is, they do not invade nearby tissue the way that cancer cells do. But, because some carcinomas in situ may become cancer, they are usually treated.
QUOTE FOR THURSDAY:
“People with an increased risk of lung cancer may consider annual lung cancer screening using low-dose CT scans. Lung cancer screening is generally offered to older adults who have smoked heavily for many years or who have quit in the past 15 years. In diagnosing tests may include: Imaging tests. An X-ray image of your lungs may reveal an abnormal mass or nodule. A CT scan can reveal small lesions in your lungs that might not be detected on an X-ray. Sputum cytology. If you have a cough and are producing sputum, looking at the sputum under the microscope can sometimes reveal the presence of lung cancer cells. Tissue sample (biopsy). A sample of abnormal cells may be removed in a procedure called a biopsy. Once your lung cancer has been diagnosed, your doctor will work to determine the extent (stage) of your cancer.”
MAYO (https://www.mayoclinic.org/diseases-conditions/lung-cancer/diagnosis-treatment/drc-20374627)
QUOTE FOR WEDNESDAY:
QUOTE FOR TUESDAY:
“Facts About Lung Cancer. LUNG CANCER is the leading cause of cancer death worldwide. AN ESTIMATED 238,340 PEOPLE will be diagnosed with lung cancer in 2023 in the U.S. 1 IN 16 PEOPLE will be diagnosed with lung cancer in their lifetime – 1 in 16 men, and 1 in 17 women.”
Lung Cancer Research Foundation (https://www.lungcancerresearchfoundation.org/lung-cancer-facts/)
QUOTE FOR MONDAY:
“In people with type 1 diabetes, the pancreas no longer makes insulin. The beta cells have been destroyed and they need insulin shots to use glucose from meals.
People with type 2 diabetes make insulin, but their bodies don’t respond well to it. Some people with type 2 diabetes need diabetes pills or insulin shots to help their bodies use glucose for energy.
Finding out you have diabetes can be overwhelming, but take a breath knowing you have a community to fall back on and the American Diabetes Association by your side to help you thrive.”.
American Diabetes Association (https://diabetes.org/)
QUOTE FOR THE WEEKEND:
“Diabetes is increasing at an alarming rate in the United States. According to the CDC’s (Centers for Disease Control) National Diabetes Statistics Report for 2022 cases of diabetes have risen to an estimated 37.3 million and one in five don’t know they have it.
The Cost of Diabetes
- In 2017, the total estimated cost of diagnosed diabetes in the U.S. was $327 billion.
- Total direct estimated costs of diagnosed diabetes increased from $188 billion in 2012 to $237 billion in 2017; total indirect costs increased from $73 billion to $90 billion in the same period (2017 dollars).
- Between 2012 and 2017, excess medical costs per person associated with diabetes increased from $8,417 to $9,601 (2017 dollars)
Remember without insulin, the body’s cells would go thru starvation, due to dehydration and destruction of body cells and tissues.
Diabetes was the seventh leading cause of death in the United States in 2017 based on the 83,564 death certificates in which diabetes was listed as the underlying cause of death.”
Diabetes Research (https://diabetesresearch.org/diabetes-statistics/)
QUOTE FOR FRIDAY:
“Diabetes is a serious, long-term condition with a major impact on the lives and well-being of individuals, families, and societies worldwide. The global diabetes prevalence in 2019 is estimated to be 9.3% (463 million people), rising to 10.2% (578 million) by 2030 and 10.9% (700 million) by 2045 [1]. Population aging is also increasing dramatically throughout the world, especially in developing countries, creating pressures on the health system as well as social security services and policies. Nowadays, many people are familiar with type 1 or type 2 diabetes mellitus, however, there is another form of diabetes that has just recently been identified, known as type 3 diabetes (T3DM). This lesser-known type manifests as insulin resistance within the brain and has major potential to impact neurocognition and contributes to the etiology of Alzheimer’s disease [AD]. AD has already been identified as the sixth leading cause of death in the United States, and the fifth leading cause of mortality in people 65 and older.”
National Library of Medicine – NIH (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246646/)
QUOTE FOR THURSDAY:
“From symptoms and treatment, to management and medication—arm yourself with the knowledge to live well with diabetes. The A1C test can be used to diagnose diabetes or help you know how your treatment plan is working by giving you a picture of your average blood glucose (blood sugar) over the past two to three months. It can identify prediabetes, which raises your risk for diabetes. It can be used to diagnose diabetes.”
American Diabetes Association (https://diabetes.org/about-diabetes)




