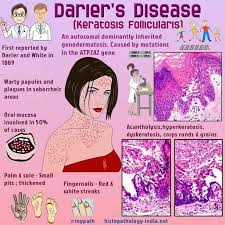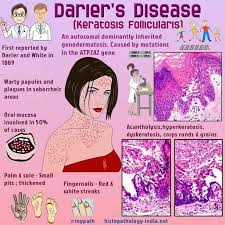

Darier disease, previously known as keratosis follicularis, is a rare autosomal dominant genodermatosis characterized by keratotic papules and longitudinal eyrthronychia; it is caused by mutations in the ATP2A2 gene, encoding a calcium pump within the endoplasmic reticulum.
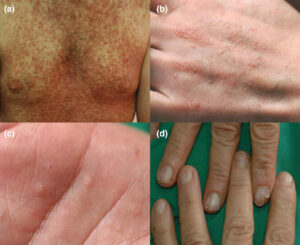
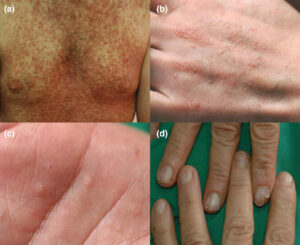
Darier disease, also known as Darier-White disease, keratosis follicularis, or dyskeratosis follicularis (MIM #124200), again know it is a rare autosomal dominant genodermatosis characterized by a persistent eruption of red-brown, keratotic papules scattered to confluent in a seborrheic distribution, nail abnormalities, pitting of palms and soles, and mucosal changes [1]. The disease usually starts around puberty and runs a chronic course with exacerbations induced by sun exposure, heat, friction, or infections.
Darier disease is exacerbated by sunlight, heat, infections, and friction. This activity reviews the clinical presentation encompassing multiple red or brown papules with hyperkeratosis, nail anomalies including longitudinal erythronychia, and mucosal changes typically surfacing around puberty and persisting throughout life. By exploring evaluation techniques and treatment modalities, this session empowers healthcare professionals to adopt a holistic approach, focusing on interdisciplinary collaboration to manage this dermatological disorder effectively. The interprofessional team’s role in assessing, diagnosing, and coordinating care for Darier disease patients is underscored, recognizing the impact of external exposures and emphasizing tailored therapeutic strategies to improve patient outcomes and quality of life. Avoid going to the dermatologist which is the worst move you could do since it will only get worse to the spread of the disease to completely over the body over years due to what exacerbates it (take the sun just alone).
This disease can be characterized by multiple dark scaly patches of itchy skin most commonly affecting the chest, back, ears, forehead, scalp, neck, and groin areas. These wart-like lesions can be foul smelling and disfiguring and has been known to affect nails and mucous membranes of the individual.
The occurrence of Darier disease is rare with the age of onset usually in the first or second decade of life. It is frequently worse in the summer with heat and humidity as major precipitating factors and can be exacerbated by sun exposure, trauma, or bacterial infections.
Review of the cause of this disease is oftentimes due to a mutation in a specific gene known as ATP2A2 which can alter the function and development of the skin. The affected parent with this gene has at least a fifty percent chance of passing it down to their children. Patients with this disease may be associated with behavioral disorders and rarely with decreased intelligence. Most patients with Darier disease have a family history of either one or both parents being affected. However, it can also present itself without any family history as well. Even though the severity fluctuates over time, Remember, Darier disease is a chronic condition that persists throughout life and is not associated with any skin cancers.
Darier disease is a rare disorder that affects all ethnic groups. The estimated prevalence ranges from 1 to 4 per 100,000 people [2-5]. In a Singaporean study, the incidence was 0.3 per 1 million people per year.
What helps diagnosing this disease :
1 A dermatology consult for the MD just to look at the skin as the first approach is the best MD to go to, the expert on skin disease diagnosing.
2. Depending on the area affected, patients with Darier disease often presents with multiple crusty and itchy patches of skin. When the scaly crusts are removed, a slit-like opening becomes visible. In areas such as nails, they are described as a sandwich of red and white bands running along the length of the nail that is thin with its characteristic V-shaped scalloping. Mucous membranes may present as white, cobblestone appearing lesions of the cheeks, palate, and gums. With the discovery of the ATP2A2 gene, skin biopsy is helpful in diagnosis through gene sequencing when suspected. SKIN BIOPSY is always helpful with diagnosing skin disease which includes tumors on the skin.
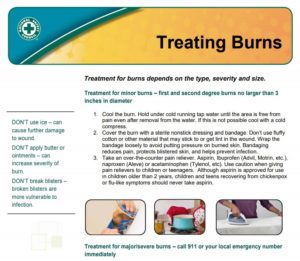
Treatments for Darier’s Disease:
This disease depends on the severity of the presented clinical symptoms.
1. For most minor cases , the disorder can be managed by using sunscreen, moisturizing lotions, avoidance of non-breathable clothing, and excessive perspiration.
2, For more severe cases of Darier’s disease, hospitalisation may be required to heal affected individuals who display frequent relapse and remit patterns. In less severe cases, signs and symptoms may clear up completely through hygienic interventions. Most patients with Darier’s disease live normal, healthy lives. Rapid resolution of rash symptoms can be complicated due to the increased vulnerability of affected skin surfaces by secondary bacterial or viral infections.
****In cases of Epidermal Staphylococcus aureus, human papillomavirus (HPV) and herpes simplex virus (HSV) infections have been reported. In these cases, topical and/or oral antibiotic/antiviral medications may need to be prescribed.****
Typical recommendations are the application of antiseptics, soaking in astringents, antibiotics, benzoyl peroxide, and topical diclofenac sodium.
If Darier’s is more localized, common treatments include:
- Topical retinoids: used to help in the reduction of hyperkeratosis, retinoids work by causing the skin cells in the top layers to die and be shed off. The common retinoids used for this disorder are:
- Adapalene
- Tazarotene gel
- Tretinoin
- Dermal abrasion
- Removal of the top layer of skin to help smooth and stimulate new growth of the skin.[21]
- Electrosurgery
- Used to help stop bleeding and remove abnormal skin growths.
- Topical corticosteroids