 ORAL CANCER RECONCONSTRUCTION SURVIVORS
ORAL CANCER RECONCONSTRUCTION SURVIVORS
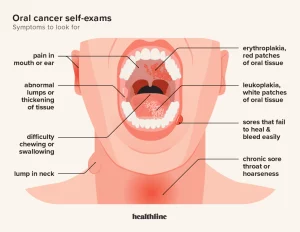
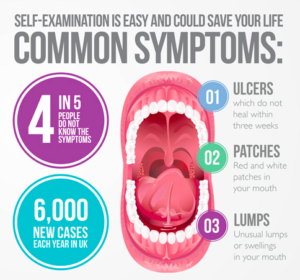 KNOW THE SYMPTOMS
KNOW THE SYMPTOMS
Most oral, head, and neck cancers begin in the cells that make up the moist tissues (mucosal surfaces) of the head and neck, including in the mouth, nose, and throat. Like other cancers, oral, head, and neck cancers occur when abnormal cells begin to grow and divide uncontrollably and form a mass, called a malignant tumor.
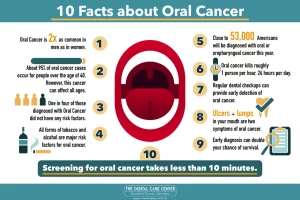
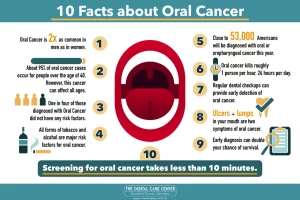
The National Cancer Institute estimates that 85 percent of oral, head, and neck cancers are linked to tobacco use. Men (age 50 or older) who use both tobacco and alcohol are at the highest risk.
Cancers of the brain, eye, thyroid, as well as the skin, bones, muscles and nerves of the head and neck are not included under the heading of “oral, head and neck” cancer.
Doctors identify oral, head, and neck cancers by the area in which the cancer begins:
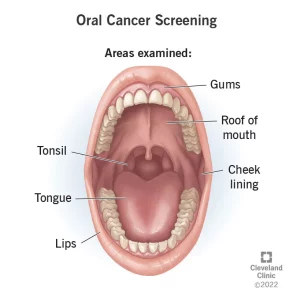
Lip and oral cavity cancer occurs on the lips, the front two-thirds of the tongue, the gums, the lining of the cheeks and lips, the floor of the mouth under the tongue, the palate, and the area behind the wisdom teeth.
Where does oral cancer affect:
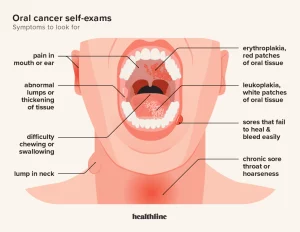
Oral cancer (mouth cancer) is the broad term for cancer that affects the inside of your mouth. Oral cancer can look like a common problem with your lips or in your mouth, like white patches or sores that bleed. Oral cancer (mouth cancer) is the most common form of head and neck cancer. It typically affects people age 60 and older. Oral cancer affects your lips and the first parts of your tongue, mouth roof and floor. It also affects your oropharynx — the last part of your tongue and roof of your mouth, your tonsils, the sides and back of your throat that can include your sinuses, and pharynx (throat). The difference between a common problem and potential cancer is these changes don’t go away. Left untreated, oral cancer can spread throughout your mouth and throat to other areas of your head and neck. Approximately 63% of people with oral cavity cancer are alive five years after diagnosis.
It can be life-threatening if not diagnosed and treated early.
When it is caught early, like other cancers is much easier for doctors to treat when caught early. Yet most people get a diagnosis when their condition is too advanced to treat effectively. If you see your dentist or doctor regularly and learn how to spot suspicious changes, you’ll have a much better shot at an early diagnosis.
Overall, about 11 people in 100,000 will develop oral cancer during their lifetime. Men are more likely than women to develop oral cancer. People who are white are more likely to develop oral cancer than people who are Black.
Risk factors in developing oral cancer include:
- Smoking. Cigarette, cigar, or pipe smokers are six times more likely than nonsmokers to develop oral cancers.
- Smokeless tobacco use. Users of dip, snuff, or chewing tobacco products are 50 times more likely to develop cancers of the cheek, gums, and lining of the lips.
- Excessive consumption of alcohol. Oral cancers are about six times more common in drinkers than in nondrinkers. Using alcohol and tobacco together increases your chances even more.
- Family history of cancer.
- Excessive sun exposure, especially at a young age. Ultraviolet radiation from the sun can cause lip cancers.
- Human papillomavirus (HPV). Certain HPV strains are etiologic risk factors for Oropharyngeal Squamous Cell Carcinoma (OSCC). Almost everyone who’s sexually active will get HPV at some point in life. A specific type of this virus is causing a growing number of otherwise healthy men under 50 to get cancers in the back of their mouths and throats from oral sex. The more people you and your partners have sex with, the bigger your risk.
- Age. Oral cancers can take years to grow. Most people find they have it after age 55. But more younger men are getting cancers linked to HPV.
- Gender. Men are at least twice as likely as women to get oral cancer. It could be because men drink and smoke more than women do.
- Poor diet. Studies have found a link between oral cancer and not eating enough vegetables and fruits.
It is important to note that over 25% of all oral cancers occur in people who do not smoke and who only drink alcohol occasionally.
The overall 5-year survival rate for patients with an early diagnosis of oral cavity and pharynx cancers is 84%. If the cancer has spread to nearby tissues, organs, or lymph nodes, the 5-year survival rate drops to 65%.
How it is diagnosed?
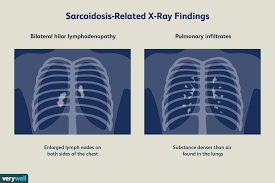
As part of your routine dental exam, your dentist will conduct an oral cancer screening exam. Your dentist knows what a healthy mouth should look like and probably has the best chance of spotting any cancer. Experts recommend getting checked every year starting at age 18, and sooner if you start smoking or having sex.
More specifically, your dentist will feel for any lumps or irregular tissue changes in your neck, head, face, and oral cavity. When examining your mouth, your dentist will look for any sores or discolored tissue as well as check for any signs and symptoms mentioned above.
A biopsy may be needed to determine the makeup of a suspicious-looking area. There are different types of biopsies and your doctor can determine which one is best.
Treatments:
It varies from person to person depending on the stage of oral cancer the person has and how advanced the cancer is.
Whether a patient has surgery, radiation, and surgery, or radiation, surgery, and chemotherapy, you need to remember it depends on the stage of cancer development. Each case is individual.
Patients with cancers treated in their early stages may have little in the way of post-treatment disfigurement. For those whose cancer is caught at a later stage, the results of surgical removal of the disease may require reconstruction of portions of their oral cavity or facial features. There may be needed adjunctive therapy to assist in speech, chewing of foods, the problems associated with the lack of salivary function, and the fabrication of dental or facial prostheses.
 ORAL CANCER RECONCONSTRUCTION SURVIVORS
ORAL CANCER RECONCONSTRUCTION SURVIVORS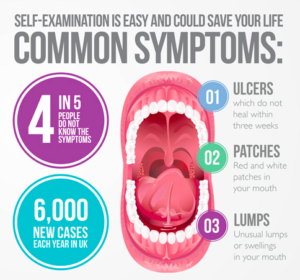 KNOW THE SYMPTOMS
KNOW THE SYMPTOMS