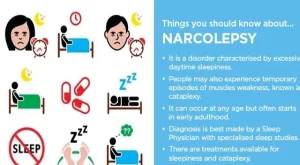
“Narcolepsy is a chronic sleep disorder, or dyssomnia. The condition is characterized by excessive daytime sleepiness (EDS) in which a person experiences extreme fatigue and possibly falls asleep at inappropriate times, such as while at work or at school.
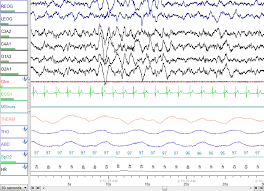
“In a recent systematic literature review and questionnaire study published in Sleep Medicine, findings showed that opioids, specifically oxycodone and codeine, were associated with improvements in self-reported narcolepsy symptoms such as disturbed nocturnal sleep and excessive daytime sleepiness. Overall, these findings suggest that opioid use could provide symptom relief in patients with narcolepsy type 1″; stated by NeurologyLive (https://www.neurologylive.com)
THEIR REFERENCES WERE:
1. Gool JK, van Heese EM, Schinkelshoek MS, et al. The therapeutic potential of opioids in narcolepsy type 1: A systematic literature review and questionnaire study. Sleep Med. 2023;109:118-127. doi:10.1016/j.sleep.2023.06.008
2. Thannickal TC, John J, Shan L, et al. Opiates increase the number of hypocretin-producing cells in human and mouse brain and reverse cataplexy in a mouse model of narcolepsy. Sci Transl Med. 2018;10(447):eaao4953. doi:10.1126/scitranslmed.aao4953
UCLA health states;
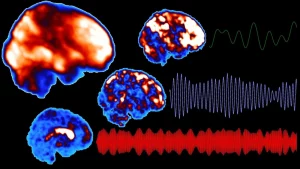
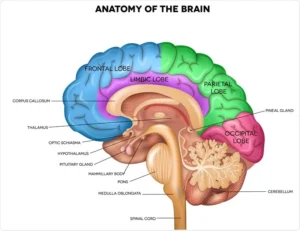
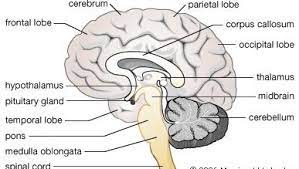
“Researchers have found both humans addicted to heroin and mice addicted to morphine develop higher numbers of hypocretin producing neurons. Morphine causes hypocretin neurons to increase their anatomical connections to pleasure related brain regions.
The annual US rate of opioid overdose deaths now exceeds 80,000, greater than the annual rates of automobile or gun deaths,” said the study’s senior author, Dr. Jerome Siegel of UCLA Health’s Jane & Terry Semel Institute for Neuroscience and Human Behavior, the UCLA Brain Research Institute and U.S. Department of Veterans Affairs.
New research led by UCLA Health has found a drug that treats insomnia works to prevent the addictive effects of the narcotic addiction effect by Morphine and other opiods. Hypocretin, also called orexin, is a peptide that is linked to mood, with hypocretin release in humans being maximal during pleasurable activities and minimal during pain or sadness. The loss of hypocretin neurons is the cause of narcolepsy, which is thought to be an autoimmune disease”
University of California – Los Angeles Health Sciences
McGregor, R., et al. (2024). Opioid-induced neuroanatomical, microglial and behavioral changes are blocked by suvorexant without diminishing opioid analgesia. Nature Mental Health. doi.org/10.1038/s44220-024-00278-2.