This is a problem with the Liver and in a nutshell it is IRON OVERLOAD!
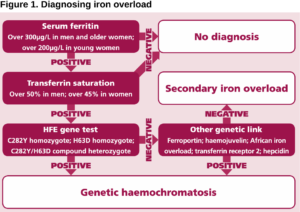
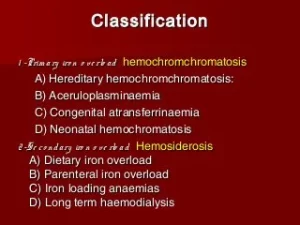
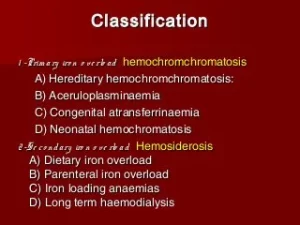
Hemochromatosis (Hemo meaning blood, Chroma meaning change in color and Osis meaning swelling) is a condition where there is abnormal accumulation of iron in the organs resulting in organ toxicity. It is the most common autosomal recessive genetic condition along with being the most common cause of severe iron overload. 75 percent of patients who have hereditary hemochromatosis are asymptomatic. The diagnosis can be made based on the clinical symptoms of the disease. Since most patients are asymptomatic, they are diagnosed when their serum iron levels are noted to be elevated during a routine chemistry screening panel. Some of the tests performed on an individual suspected with hemochromatosis include genetic testing to test for HFE mutations, transferrin saturation levels, hepatic iron concentration, and serum ferritin studies. Imaging studies such as a chest radiography and echocardiography might be beneficial to help evaluate cardiac disease in patients with hemochromatosis.
Early diagnosis is important in hemochromatosis, like in most every other diagnosis.
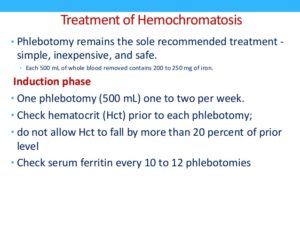
The aim of therapy is to remove iron before it causes irreversible parenchymal damage. Once the diagnosis is confirmed, it is treated by phlebotomy to maintain normal iron stores and rid the body of excess iron. Chelation therapy uses agents such as deferoxamine, deferiprone, or deferasirox. Surgery may be required if there is end stage liver disease or severe arthropathy. In the United States, hereditary hemochromatosis is found in 1 of 200 to 500 individuals. Most of these cases are seen in individuals of northern European origin. It has the same prevalence in Australia, Europe, and other western countries. The highest prevalence is among individuals of Celtic origin and less among those of African descent.
Symptoms would be:
1.) Fatigue and 2 types of fatigue, that would be:
Physical fatigue occurs when there is transient inability to achieve peak physical performance.
Mental fatigue is the temporary inability to maintain optimal cognitive performance. It is a common and non-specific symptom that can be seen in stress, overwork, depression, boredom, anemia, inadequate sleep, malnutrition, pregnancy, infections, and more. It can manifest as somnolence in patients.
2.) Impotence in patients with hemochromatosis is due to a result of hypogonadism. Hypogonadism can occur in hemochromatosis patients due to pituitary or testicular iron deposition.
3.) Arthropathy that’s a disease of a joint. In arthropathy, there can be joint pain, stiffness, swelling, and decreased range of motion. Patients can see this occuring because of the accumulation of iron in the joint tissues. The most commonly affected joints are the knees, feet, wrists, neck, back, metacarpophalangeal joints, and proximal interphalangeal joints.
4.) It has been observed that 62 percent of patients with hemochromatosis experience partial loss of body hair. The most commonly affected area is the pubic area. Approximately 12 percent of patients experience total body hair loss. In some patients, the thinning and loss of hair may be reversed through therapy.
5.) Koilonychia refers to spoon nails where the nails are abnormally thin and have lost their convexity resulting in flat or concave nails. Causes of koilonychia include iron deficiency anemia and it can be seen in 25 to 50 percent of these patients.
6.) Skin Hyperpigmentation or Bronzing of the skin refers to darkening of the skin. It is due to the combination of melanin and iron deposition which is characteristic. It is one of the classic triad symptoms with the other two being cirrhosis and diabetes in the late stages of the disease. This usually occurs only when the total iron content in the body is more than 5 times the normal levels.
7.) Amenorrhea refers to the absence of menstruation in females who are in their reproductive age.
8.) In the heart it can cause the following: Atrial flutter is a problem with the way your heart beats. Such problems, whether in the rhythm or speed of the heartbeat, are known as arrhythmias. Heart Failure is the other.
In addition to these symptoms it can also cause problems with the spleen, adrenal glands, pituitary gland, gallbladder or thyroid.
For helping in possible PREVENTION of this diagnosis and most others stay as healthy as possible and get yearly check ups to pick up this or any other diagnosis EARLY!! In so many cases of diseases the early picked up or diagnosed the better the results turn out in most cases. When a disease just start in your body is being treated compared to late in the disease higher the odds will resolve or you will last longer with a better quality of life, just like with so many other diseases!