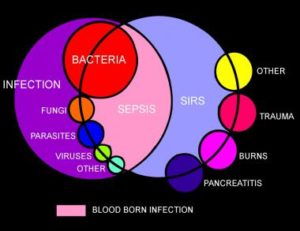
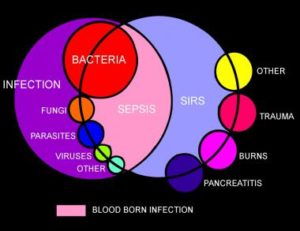
Sepsis is a potentially dangerous or life-threatening medical condition, found in association with a known or suspected infection (usually caused by but not limited to bacteria).
1.What causes sepsis?
In sepsis the infection has spread from a local area of the body with spreading into a systemic infection, this means the infection is in the blood stream now. So you have gone from a infection in one spot (local) now in another area of the body, the blood stream (now a systemic infection), that goes to every tissue of our body bringing the infection to effect anywhere in our body from 2 or several organs in the body to death if not treated.
Bacterial infections are the most common cause of sepsis. Sepsis can also be caused by fungal, parasitic, or viral infections. The source of the infection can be any of a number of places throughout the body. Common sites and types of infection that can lead to sepsis include:
- The abdomen—An inflammation of the appendix (appendicitis), bowel problems, infection of the abdominal cavity (peritonitis), and gallbladder or liver infections. If spreads the peritoneum (The serous membrane lining the cavity of the abdomen and covering the abdominal organs.) Through the membrane the infection spreads to a abdominal organ or organs.
- The central nervous system—Inflammation or infections of the brain or the spinal cord, easy to get into the bloodstream.
- The lungs—Infections such as pneumonia, our lungs give our blood oxygen so easy for the infection to spread into our bloodstream.
- The skin—Bacteria can enter skin through wounds or skin inflammations, or through the openings made with intravenous (IV) catheters (tubes inserted into the body to administer or drain fluids). Conditions such as cellulitis (inflammation of the skin’s connective tissue) can cause sepsis.
- The urinary tract (kidneys or bladder)—Urinary tract infections are especially likely if the patient has a urinary catheter to drain urine.
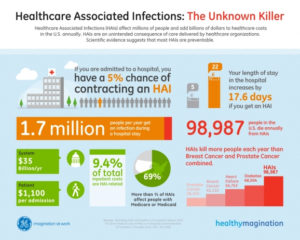
Sepsis can strike anyone, but their are those at particular risk.
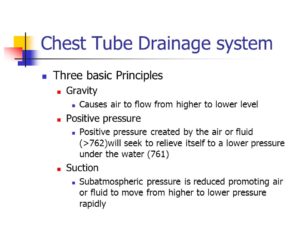
Sepsis has to show signs and symptoms to fulfill at least two of the following criteria of a systemic inflammatory response syndrome (SIRS):
- elevated heart rate (tachycardia) >90 beats per minute at rest, your heart is fighting this infection.
- body temperature either high (>100.4 F or 38 C) usually the case at first or low (<96.8 F or 36 C), the body now
- increased respiratory rate of >20 breaths per minute or a reduced PaCO2 (partial pressure of carbon dioxide in arterial blood level)
- abnormal white blood cell count (>12,000 cells/µL or <4,000 cells/µL or >10% bands [an immature type of white blood cell])
2.Who is at risk for sepsis?
- People with weakened immune systems
- Patients who are in the hospital
- People with pre-existing infections or medical conditions
- People with severe injuries, such as large burns or bullet wounds
- People with a genetic tendency for sepsis
- The very old or very young.
3.What are the symptoms of sepsis?
- Decreased urine output
- Fast heart rate
- Fever
- Or the opposite Hypothermia (very low body temperature)
- Shaking
- Chills
- Warm skin or a skin rash
- Confusion or delirium
- Hyperventilation (rapid breathing)A person may have sepsis if he or she has:
4.How is sepsis diagnosed?
- A high or low white blood cell count
- A low platelet count
- Acidosis (too much acid in the blood); in the hospital what is checked is lactic acid blood level.
- A blood culture that is positive for bacteria
- Abnormal kidney or liver functionm
5.TREATMENT:
- Patients who meet the above criteria on symtoms have sepsis and are also termed septic. In acute hospitals if 2 of these infections are present in the patient a “Septic Code” is called to get pt on antibiotics 2 usually that include Vancomycin, with IVFs started continuously, blood tests including bacterial culture x2, to the ICU where closely monitored, on telemetry. Keep the pt continuously clean.
- The most important intervention in sepsis is quick diagnosis and prompt treatment. Patients diagnosed with severe sepsis are usually placed in the intensive care unit (ICU) of the hospital for special treatment. The doctor will first try to identify the source and the type of infection, and then administer antibiotics to treat the infection. (Note: antibiotics are ineffective against infections caused by viruses; if anything what is used is antiviral medications.)
- The doctor also administers IV fluids to prevent blood pressure from dropping too low. In some cases, vasopressor medications (which constrict blood vessels) are needed to achieve an adequate blood pressure. Some patients are given new drug therapies, such as activated protein C (APC). And finally, if organ failures occur, appropriate supportive care is provided (for example, dialysis for kidney failure, mechanical ventilation for respiratory failure, etc.).
- Commonly what is used when initially sepsis is diagnosed is Vancomycin with other antibiotics like Imipenum, Cefepime, and others depending on what the blood culture results show as the microorganism. Antibiotics with Sepsis and SIRS is caused by a bacterial infection (many times it is).
SIRS –
SIRS with a suspected source of infection is termed sepsis. Confirmation of infection with positive cultures is therefore not mandatory, at least in the early stages. Sepsis with one or more end-organ failures is called severe sepsis, and hemodynamic instability despite intravascular volume repletion is called septic shock. Together they represent a physiologic continuum with progressively worsening balance between pro and anti-inflammatory responses of the body.
The American College of Chest Physicians/Society of Critical Care Medicine-sponsored sepsis definitions consensus conference also identified the entity of multiple organ dysfunction syndrome (MODS) as the presence of altered organ function in acutely ill septic patients such that homeostasis is not maintainable without intervention.
Objectively, SIRS is defined by the satisfaction of any two of the criteria below:
-
Body temperature over 38 or under 36 degrees Celsius. (100.4 Farenheit down to 96.8° Fahrenheit)
-
Heart rate greater than 90 beats/minute
-
Respiratory rate greater than 20 breaths/minute or partial pressure of CO2 less than 32 mmHg
-
Leukocyte (white blood cell) count greater than 12000 or less than 4000 /microliters or over 10% immature forms or bands.
Treatment:
Treatment focuses on the underlying cause. Early care to treat for septic shock is critical in patients suspected of infection and hemodynamic instability.
Routine prophylaxis, including deep vein thrombosis (DVT) and stress ulcer prophylaxis, should be initiated when clinically indicated in severely ill bed-ridden patients, especially if they require mechanical ventilation. Long-term antibiotics, when clinically indicated, should be as narrow spectrum as possible to limit the potential for superinfection (suggested by a new fever, a change in the white blood cell [WBC] count, or clinical deterioration). Unnecessary vascular catheters and Foley catheters should be removed as soon as possible.
SIRS is a syndrome, not a disease. Treatment of SIRS should focus on possible inciting causes. As the causes of SIRS include a wide range of disorders (eg, acute myocardial infarction, community-acquired pneumonia, [9] pancreatitis), the appropriate interventions will likewise differ from patient to patient.