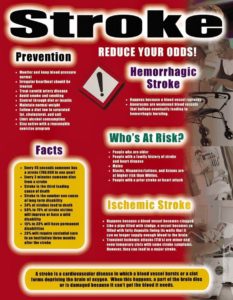
Signs and Symptoms of a stroke happening:
Symptoms of stroke include trouble walking, speaking, and understanding, as well as paralysis or numbness of the face, arm, or leg.
People may experience the following:
Muscular: difficulty walking, paralysis with weak muscles, problems with coordination, stiff muscles, overactive reflexes, or paralysis of one side of the body
Visual: blurred vision, double vision, sudden visual loss, or temporary loss of vision in one eye
Whole body: balance disorder, fatigue, or lightheadedness
Speech: difficulty speaking, slurred speech, or speech loss
Sensory: pins and needles or reduced sensation of touch
Facial: muscle weakness or numbness
Limbs: numbness or weakness
Also common: difficulty swallowing, headache, inability to understand, mental confusion, numbness, or rapid involuntary eye movement
What is done for a stroke regarding diagnostic tooling:
To determine the most appropriate treatment for your stroke, your emergency team needs to evaluate the type of stroke you’re having and the areas of your brain affected by the stroke. They also need to rule out other possible causes of your symptoms, such as a brain tumor or a drug reaction. Your doctor may use several tests to determine your risk of stroke, including:
CT scan of brain tissue damaged by stroke
Cerebral angiogram A cerebral angiogram showing a carotid aneurysm due to a stroke.
Physical examination. Your doctor will ask you or a family member what symptoms you’ve been having, when they started and what you were doing when they began. Your doctor then will evaluate whether these symptoms are still present.
Your doctor will want to know what medications you take and whether you have experienced any head injuries. You’ll be asked about your personal and family history of heart disease, transient ischemic attack or stroke.
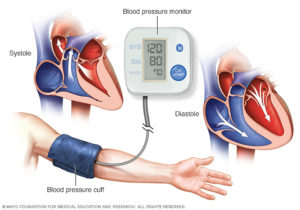
Your doctor will check your blood pressure and use a stethoscope to listen to your heart and to listen for a whooshing sound (bruit) over your neck (carotid) arteries, which may indicate atherosclerosis. Your doctor may also use an ophthalmoscope to check for signs of tiny cholesterol crystals or clots in the blood vessels at the back of your eyes.
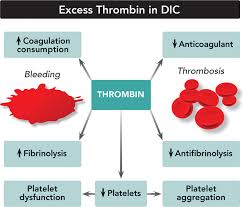
Blood tests. You may have several blood tests, which tell your care team how fast your blood clots, whether your blood sugar is abnormally high or low, whether critical blood chemicals are out of balance, or whether you may have an infection. Managing your blood’s clotting time and levels of sugar and other key chemicals will be part of your stroke care.
Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed image of your brain. A CT scan can show a hemorrhage, tumor, stroke and other conditions. Doctors may inject a dye into your bloodstream to view your blood vessels in your neck and brain in greater detail (computerized tomography angiography). The goal is if the CT scan determined the stroke to be a ischemic stroke start rtpa a drug IV if the symptoms of the stroke started in the past 3 hrs if not treat it another way OR if the stroke is determined to be hemorrhagic than its the OR. Will go into treatment in more detail in Part III tomorrow.
Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and magnets to create a detailed view of your brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiography, or magnetic resonance venography).
Carotid ultrasound. In this test, sound waves create detailed images of the inside of the carotid arteries in your neck. This test shows buildup of fatty deposits (plaques) and blood flow in your carotid arteries.
Cerebral angiogram. In this test, your doctor inserts a thin, flexible tube (catheter) through a small incision, usually in your groin, and guides it through your major arteries and into your carotid or vertebral artery. Then your doctor injects a dye into your blood vessels to make them visible under X-ray imaging. This procedure gives a detailed view of arteries in your brain and neck.
Echocardiogram. An echocardiogram uses sound waves to create detailed images of your heart. An echocardiogram can find a source of clots in your heart that may have traveled from your heart to your brain and caused your stroke.
You may have a transesophageal echocardiogram. In this test, your doctor inserts a flexible tube with a small device (transducer) attached into your throat and down into the tube that connects the back of your mouth to your stomach (esophagus). Because your esophagus is directly behind your heart, a transesophageal echocardiogram can create clear, detailed ultrasound images of your heart and any blood clots.
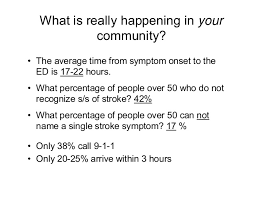
In reality going to an ER room if the pt comes suspected of a stroke and has symptoms or not than nationally in America the hospitals are to do the following:
-A neuro assessment should be done in 10 minutes by the doctor.
-A CT SCAN ordered and pt sent off for the CT SCAN test and done within 25 minutes.
-The CT SCAN read and interpreted by the radiologist / neuro doctor within 45 minutes. At this point it tells the MD if the pt has a blockage or a hemmorage in the brain that caused the stroke. Remember a ischemic stroke and hemmoragic stroke are treated differently.
We’ll get into treatment tomorrow in Part III Treatment of a stroke.