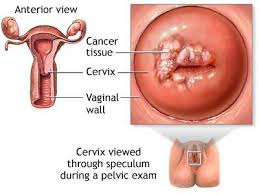
Part II Cervical Cancer Awareness Month-Risk Factors, Symptoms of it, Signs of advanced cervical cancer!
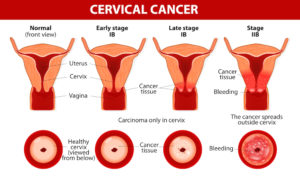
Cervical Cancer. Carcinoma of Cervix. Malignant neoplasm arising from cells in the cervix uteri. Vaginal bleeding. Vector diagram
Cervical cancer risk factors
GENERAL
- Pregnancy: Women who have had three or more full-term pregnancies, or who had their first full-term pregnancy before age 17, are twice as likely to get cervical cancer.
GENETICS
- Family history: Women with a sister or mother who had cervical cancer are two to three times more likely to develop cervical cancer.
LIFESTYLE
- Sexual history: Certain types of sexual behavior are considered risk factors for cervical cancer and HPV infection. These include: sex before age 18, sex with multiple partners and sex with someone who has had multiple partners. Studies also show a link between chlamydia infection and cervical cancer.
- Smoking: A woman who smokes doubles her risk of cervical cancer.
- Oral contraceptive use: Women who take oral contraceptives for more than five years have an increased risk of cervical cancer, but this risk returns to normal within a few years after the pills are stopped.
OTHER CONDITIONS
- Weakened immune system: In most people with healthy immune systems, the HPV virus clears itself from the body within 12-18 months. However, people with HIV or other health conditions or who take medications that limit the body’s ability to fight off infection have a higher risk of developing cervical cancer.
- Diethylstilbestrol (DES): Women whose mothers took DES, a drug given to some women to prevent miscarriage between 1940 and 1971, have a higher risk of developing cervical cancer.
- HPV: Though HPV causes cancer, having HPV does not mean you will get cancer. The majority of women who contract HPV clear the virus or have treatment so the abnormal cells are removed. HPV is a skin infection, spread through skin-to-skin contact with a person who has the virus.
Additional facts about HPV:
- There are more than 100 types of HPV, 30-40 of which are sexually transmitted.
- Of these, at least 15 are high-risk HPV strains that can cause cervical cancer. The others cause no symptoms or genital warts.
- Up to 80 percent of women will contract HPV in their lifetime. Men get HPV, too, but there is no test for them.
- A healthy immune system will usually clear the HPV virus before there is a symptom, including the high-risk types of HPV.
- Only a small percentage of women with high-risk HPV develop cervical cancer.
Understanding risk factors:
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer. Not having risk factors doesn’t mean that you will not get cancer. If you think you may be at risk, you should discuss it with your doctor.
Regarding symptoms of cervical cancer:
In most cases, cervical cancer does not cause noticeable symptoms in the early stages of the disease. Routine Pap screening is important to check for abnormal cells in the cervix, so they can be monitored and treated as early as possible. Most women are advised to get a Pap test starting at age 21.
The Pap test is one of the most reliable and effective cancer screening methods available, and women should have yearly exams by an OB-GYN. However, the Pap test may not detect some cases of abnormal cells in the cervix. The HPV test screens women for the high-risk HPV strains that may lead to cervical cancer. It is approved for women over age 30.
Although screening methods are not 100 percent accurate, these tests are often an effective method for detecting cervical cancer in the early stages when it is still highly treatable. Talk with your doctor about which type of cervical cancer screening is right for you.
When present, common symptoms of cervical cancer may include:
- Vaginal bleeding: This includes bleeding between periods, after sexual intercourse or post-menopausal bleeding.
- Unusual vaginal discharge: A watery, pink or foul-smelling discharge is common.
- Pelvic pain: Pain during intercourse or at other times may be a sign of abnormal changes to the cervix, or less serious conditions.
All of these cervical cancer symptoms should be discussed with your doctor.
Signs of advanced stages of cervical cancer:
Cervical cancer may spread (metastasize) within the pelvis, to the lymph nodes or elsewhere in the body. Signs of advanced cervical cancer include:
- Weight loss
- Fatigue
- Back pain
- Leg pain or swelling
- Leakage of urine or feces from the vagina
- Bone fractures
QUOTE FOR FRIDAY:
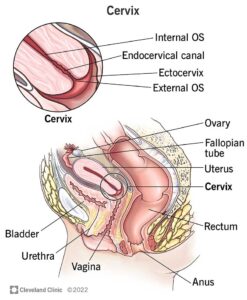
“Cervical cancer is a growth of cells that starts in the cervix. The cervix is the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus, also called HPV, play a role in causing most cervical cancers. HPV is a common infection that’s passed through sexual contact. When exposed to HPV, the body’s immune system typically prevents the virus from doing harm. In a small percentage of people, however, the virus survives for years. This contributes to the process that causes some cervical cells to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.”
MAYO CLINIC (Cervical cancer – Symptoms and causes – Mayo Clinic)
Part I Cervical Cancer Awareness Month & Signs to watch out for!
What is Cervical Health Awareness Month?
The United States Congress designated January as Cervical Health Awareness Month. During January, NCCC and its many local chapters across the country highlight issues related to cervical cancer, HPV disease and the importance of early detection. More than 40 years ago cervical cancer was a major cancer death risk for women. With the development of pap tests and in-depth recognition of warning signs those numbers are dropping significantly. We still aren’t completely safe however, as many thousands of women are still affected by cervical cancer every year.
Cervical Cancer is today’s issue. Through National Cervical Cancer Coalition with Dr. Warner Huh stated the following information about today’ topic:
Cervical cancer screening used to all be so simple==PREVENTION. Women were told just go for your annual Pap but now we have new tests to screen for cervical cancer, plus updated guidelines that—for most women—mean routine screening is done every few years rather than annually. Dr. Warner Huh of the University of Alabama, Birmingham sorts out the new landscape of Pap and HPV tests.
Human papillomavirus, or HPV, is a common sexually transmitted infection. So common that most (~80%) sexually active people will be infected with HPV at some point.
Cervical cancer begins in the cervix, the narrow organ at the bottom of the uterus that connects to the vagina. The cervix dilates during childbirth to allow for passage of a baby.
Picking up on risk factors and warning signs could save an individual from a lifetime of suffering. These include whether or not you’ve contracted HPV, if you eat a whole diet, have used birth control, have HIV, smoke cigarettes, or if it’s just in your genetics.
Here are some signs to watch out for:
Leg Pain – Some women exhibiting early stages of cervical cancer experience swelling and pain in the leg. When the cervix swells it can lead to an obstructed blood flow, which eventually causes the leg to swell and gives a sore, painful sensation. This may be a sign of early cervical cancer.
Vaginal discharge colored with blood – It’s normal for a woman to experience small amounts of clear discharge without color or odor. However, bloody, dark, or smelly discharge is usually a sign of infection. But sometimes, it’s a sign of cervical or endometrial cancer.
Abnormal vaginal bleeding – More than 90% of women diagnosed with endometrial cancer experience irregular bleeding. If you have already undergone menopause, any bleeding — spotting included — should be evaluated. Haven’t gone through menopause yet? See your doctor if you experience bleeding between periods, heavy bleeding or bleeding during sex.
Discomforting Urination – Keeping track of urination can help reveal the presence of cervical cancer in several ways. The most immediately obvious and prevalent symptom is discomfort while urinating. You may experience burning, stinging, or a tight sensation. This is another symptom to see a doctor about either way.
Irregular Urination – The appearance of the urine and urinary habits can also be symptoms of cervical cancer. If you notice strange changes in the frequency of your urine, loss of bladder control (incontinence) or a discoloration – especially with blood – seek the input of a medical professional.
Irregular Menstrual Cycles – There should be some level of consistency when it comes to monthly periods. If time, frequency, or any other changes disrupt the regular routine, it can also be a sign that you’re at a much higher risk for cancer and will require regular screenings.
Uncomfortable Sex – Painful intercourse, otherwise known as dyspareunia, is another discomforting side effect of cervical cancer. There are several possible reasons for this symptom to develop, as is the case with many of the symptoms on this list. This symptom is most commonly linked to conditions that require medical attention, however, so it shouldn’t be ignored.
Pain in the pelvis or abdominal area – Abdominal pain or discomfort — including gas, indigestion, pressure, bloating, and cramps — can signal ovarian cancer. And, constant pelvic pain or pressure can be a sign of endometrial cancer.
Back Pain – Back pain is common, affecting around 80 percent of the population, and it can happen for a wide variety of reasons, but if accompanied with other symptoms from the list, go for a medical check-up.
Stayed tune to Part II of Cervical Awareness Month tomorrow!
QUOTE FOR THURSDAY:
“The cervix is the lower, narrow end of the uterus that connects the uterus to the vagina. It is made up of the internal OS (the opening between the cervix and the upper part of the uterus), the endocervix (the inner part of the cervix that forms the endocervical canal), the ectocervix (the outer part of the cervix that opens into the vagina) and the external OS (the opening between the cervix and vagina).”
National Cancer Institute – NIH (Definition of cervix – NCI Dictionary of Cancer Terms – NCI)
Know what the cervix is and why this month!
Where is your cervix located?
Your cervix is an important part of your reproductive anatomy. Your cervix is located inside your pelvic cavity, anywhere from 3 to 6 inches inside your vaginal canal. It begins at the base of your uterus and extends downward onto the top part of your vagina. This place where your cervix bulges onto the uppermost part of your vagina is called your ectocervix.
Your vagina, cervix and uterus are located behind your bladder and urethra (organs that allow you to pee) and in front of your rectum and anus (organs that allow you to poop).
What does your cervix look like?
The word “cervix” comes from the Latin word meaning “neck.” Like a neck, your cervix is shaped roughly like a cylinder or tube and connects important body parts. While your neck connects your head to the rest of your body, your cervix connects your uterus to your vagina. Your cervix is wider in the middle and narrows at both ends, where it opens into your uterus (top) and vagina (bottom).
Your cervix consists of the following parts:
- Internal OS: The opening that leads to your uterus. Your provider may refer to your internal OS during pregnancy.
- Endocervical canal: A tunnel that extends from your Internal OS to your ectocervix.
- Ectocervix: The part of your cervix that bulges onto the top of your vagina.
- External OS: The opening that leads to your vagina.
Your cervix is a muscular, tunnel-like organ. It’s the lower part of your uterus, and it connects your uterus and vagina. Sometimes called the “neck of the uterus,” your cervix plays an important role in allowing fluids to pass between your uterus and vagina. It enables a baby to leave your uterus so that it can travel through your vagina (birth canal) during childbirth. The cervix is also a common site for cell changes that may indicate cancer.
Getting regular Pap smears allows your provider to screen for irregularities that may be signs of disease.
Who has a cervix?
People who are designated female at birth (DFAB) have a cervix. DFAB people include cisgender women — people who are DFAB and identify as women — and some transgender men and nonbinary individuals. Some intersex individuals have cervixes, too.
What is the functions of your cervix?
Your cervix is a passage that allows fluids to flow inside and out of your uterus. It’s also a powerful gatekeeper that can open and close in ways that make pregnancy and childbirth possible.
Your cervix plays important roles in the following:
- Menstruation: The period blood you shed each month as part of your menstrual cycle has to pass from your uterus and through your cervix before exiting your vagina.
- Pregnancy: During penis-in-vagina sex, or intercourse, your partner may ejaculate (release) sperm into your vagina. The sperm has to travel through your cervix to reach your uterus and fallopian tubes to fertilize an egg.
- Fertility: Your cervical mucus plays a role in how easily you can become pregnant. Around ovulation (when your body releases an egg), your cervix secretes mucus that’s thinner and less acidic than usual, making it easy for sperm to pass through to your uterus. As a result, sperm can reach your egg and fertilize it more easily.
- Vaginal delivery: Your cervix controls when a baby exits your uterus during childbirth. During pregnancy, your cervix secretes a mucus plug that seals entry to your uterus. Once it’s time for the baby to be born, the mucus plug dissolves, and your cervix becomes softer and thinner. Your cervix widens (dilates) so that the baby can exit your uterus. Your provider can estimate how long it will take for your baby to be born based on how much your cervix has dilated.
- Protecting your uterus: Your cervix prevents objects inserted into your vagina, such as tampons or diaphragms, from slipping inside your uterus.
The place where the endocervical canal overlaps with the ectocervix is called the transformation zone (TZ). The TZ is the part of your cervix where cell changes happen most. It’s the most common site for abnormal cells to grow in your cervix, indicating conditions like cervical dysplasia or cervical cancer.
How big is your cervix?
Your cervix is about an inch long. Cervical sizes vary, though. Generally, your cervix is larger if you’ve given birth. The cervix is larger among people in their reproductive years than those who’ve gone through menopause. Your cervix gets significantly shorter during childbirth to allow a baby to easily exit your uterus and enter your vagina.
Can you touch your cervix?
Yes, depending on the timing of your menstrual cycle. If you insert your longest finger into your vaginal canal, you should eventually reach a barrier preventing your finger from sliding in further. This barrier is your cervix. It may feel firm and tight, or it may feel soft and spongy. The location and texture of your cervix change depending on whether or not you’re ovulating. It’s the softest and hardest to reach during ovulation.
Take care that you only attempt to touch your cervix when you’ve washed your hands thoroughly with mild soap and warm water. Otherwise, you could expose your cervix to bacteria and cause infection.
What is your cervix made of?
Your cervix consists of strong fibromuscular tissue. Two main types of cells line your cervix:
- Glandular cells: These cells line the endocervical canal, the innermost part of your cervix.
- Squamous cells: These cells cover the ectocervix, the outermost part of your cervix, and your vagina.
These different cell types meet at the TZ, where cell changes frequently take place. This area is of particular interest to your provider during screenings for cervical cancer.
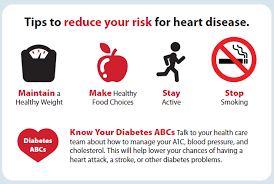
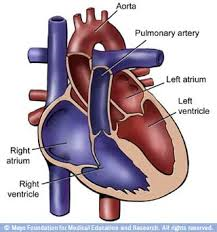
An eye opener on Heart Disease that should be rare & cured.
It is still the number one killer even greater than cancer in both men and women today. This disease should be rare; do to a lot of cardiac disease it is inflicted upon humans through being overweight through just bad healthy habits practiced. Obesity can cause diabetes II, heart disease, high blood pressure, and more. High blood pressure is called the “silent killer” because it often has no warning signs or symptoms, and many people don’t realize they have it. That’s why it’s important to get your blood pressure checked regularly. The good news is that you can take steps to prevent high blood pressure, or to treat it if it is already high.
What we can do is make some changes in our living. We westerners create an increase in diabetes, heart disease and some cancers. AMERICA WE NEED TO WAKE UP AND MAKE A CHANGE. TO THE MAIN CULPRITES we are talking about sugars and fat (OUR DIET). GLUCOSE and LIPIDS!. The typical American diet is consisted and loaded with sugar and fats. Lack of exercise and stress doesn’t help the situation. Get peace of mind through again making changes in your life if you are striving to become healthier. Let’s look at cholesterol = 2 types HDL and LDL. LDL is the bad cholesterol. Know if your LDL is type A or type B. If you have a high HDL level and a low LDL that is good but ask your doctor to see if you can get a blood test checking both type A and type B of your cholesterol that will give you the knowledge if you need to take an action. Go to CDC.org to see the different number ranges of both men and women on their levels and more. Just knowing your cholesterol level isn’t enough but does give the doctor some direction. Knowing if your type A or type B LDL helps even more with knowing your risk of heart disease.
Cholesterol only becomes a problem if the LDL gets too high with high pattern type B which is worse with stress and smoking and processed foods in high amounts eaten. Particles called lipoproteins carry cholesterol in the blood. There are two kinds of lipoproteins you need to know about: LDL and HDL. The plasma lipoprotein particles classified under high-density (HDL) and low-density (LDL) lipoproteins enable fats to be carried in the blood stream.
-Low-density lipoproteins (LDL) cholesterol make up the majority of the body’s cholesterol. LDL is known as “bad” cholesterol because having high levels can lead to a buildup in the arteries and result in heart disease.
-High-density lipoproteins (HDL) cholesterol absorb cholesterol and carry it back to the liver, which flushes it from the body. High levels of HDL, or “good” cholesterol, reduce the risk of heart disease and stroke.
Apolipoprotein A1 (apoA1) is the major protein of high-density lipoprotein (HDL), and apoB is among the major proteins of very low-, low- (LDL), and intermediate-density lipoproteins. Because of their associations with the respective lipoproteins, apoA1 is inversely and apoB is positively associated with cardiovascular risk (2). In fact, evidence suggests that apoA1 and apoB are better predictors of heart disease risk than are HDL and LDL cholesterol levels (3-5). Apolipoproteins may also offer advantages over lipoprotein cholesterol measurements because they are direct measurements, whereas LDL, for example, is calculated from other lipoproteins from a fasting blood sample.
You can take several steps to maintain a normal cholesterol level.
- Get a blood test.
- Eat a healthy diet.
- Maintain a healthy weight.
- Exercise regularly.
- Don’t smoke.
- Treat high cholesterol.
Heart disease what is it? Your arteries can get stretched in high blood pressure and it puts the arteries at risk for an auto immune response which allows LDL particles to go in these stretched out areas causing build up of bad cholesterol in the arteries and imbeds fat causing the placque build up = narrowing of the arteries.
We need to reduce inflammation in the arteries. To prevent, reduce, and treat heart disease if already diagnosed with. Reduce all sugars, cut back on fatty foods, exercise daily, increase of your whole grains, fresh fruits, and vegetables. We need to use all 4 food groups but eat the healthy ones in the right portions. Which I can provide to you later how to go about this.
In the United States, the most common type of heart disease is coronary artery disease (CAD), which leads many to heart attacks. You can greatly reduce your risk for CAD through lifestyle changes and, in some cases, medication. CAD consists of cholesterol and placque build up, even tar if a smoker, that can be deadly in time with blocking the arteries called atherosclerosis. This in time left untreated can lead to a heart attack or even silent heart attack. CAD also is the brittling of the arteries causing narrowing of the arteries called arteriosclerosis. Here it is the ending result is the blood supply is affected in not getting enough oxygen throughout our body to our tissues.
Coronary artery disease can cause a heart attack. If you have a heart attack, you are more likely to survive if you know the signs and symptoms, call 9-1-1 immediately, and get to a hospital quickly. People who have had a heart attack can also reduce the risk of future heart attacks or strokes by making lifestyle changes and taking medication. Don’t put off the chest pain or discomfort in the chest or pain down the L arm for if your right you want to prevent the heart attack before it occurs and if you already had an attack the sooner treated the better. Reperfusion of blood to the heart is the KEY in treatment. Chest pain to the heart is lack of oxygen getting to the heart tissue=ischemia. We alone can’t treat it but we can prevent it before CAD even sets in through good health practices daily, healthy dieting daily and balancing rest with exercise daily.
Look at our diet alone in America: Take the elements that are in our food=Sugars or Carbohydrates or Fats. Simple CHO likes bread, rice, pasta along with fats and complex sugars all convert to simple sugars in the stomach and when it goes through digestion and the simple sugar reaches the blood stream filling it up with sugar which first does get utilized to our tissues and cells but if still extra sugar in the blood stream that sugar has to go somewhere which is by filling up the liver with it. In the liver the glucose gets converted from active sugar=glucose to glycogen=inactive sugar that stores in this organ. This is so if and when the body needs extra sugar for energy in our body and we don’t eat the inactive glucose glycogen will get released back into the blood stream and change to glucose and be used. Since we eat so much in America it usually isn’t the case. Obesity is so large in our country and this is why. When it reaches full and can’t store anymore still this glucose extra glucose in the blood stream has to go somewhere. So now the glucose gets stored in our fatty tissue=weight gain. This is what you see with eating through on a regular basis day in & day out too much food compared to the activity or exercise you get for the day. If no daily exercise then your fat storage build up is high=weight gain.
How do we go about preventing CAD and getting healther. Well see if this makes sense to you, it did to me. First, genetic abnormalities contribute to the risk for certain types of heart disease, which in turn may lead to heart failure. However, in most instances, a specific genetic link to heart failure has not been identified.
SO THE KEY TO PREVENTION OF CAD IS TO LIVE AS HEALTHY AS POSSIBLE IN YOUR ROUTINE HABITS, YOUR DIETING OF THE 4 FOOD GROUPS, MAINTAINING YOUR WEIGHT IN A THEREPEUTIC RANGE (look as calculating BMI online for free to find out what your weight range for your height is), and BALANCING REST WITH EXERCISE TO HELP DECREASE THE CHANCE OF GETTING HEART FAILURE.
QUOTE FOR MONDAY:
“Don’t know how to celebrate here are some things to avoid in doing to stay healthy:
What to avoid during New Year’s Eve party?
In order to understand how to celebrate the New Year in a healthy way, make sure to stay away from these things:
- Excess alcohol consumption: “Drinking too much can cause dehydration, impaired judgment, and hangovers,” says general physician Dr Simon Grant. Always stay within safe limits. That means don’t drink more than one or two glasses of alcohol.
- Overindulging in unhealthy foods: Avoid high-sugar and high-fat foods that can cause blood sugar spikes, digestive issues, and lethargy.
- Lack of hydration: Ensure you drink plenty of water, especially if you are consuming salty snacks or alcohol.
- Smoking and secondhand smoke: Avoid environments where smoking is prevalent. Both active and passive smoking can harm your respiratory health.
- Skipping meals before the party: Don’t starve yourself to indulge during the New Year’s Eve party. This can lead to overeating as well as stomach discomfort.”
Health Shots (www.healthshots.com How to celebrate the New Year in a healthy way? Know 12 tips | HealthShots)
What to do on New Years Eve if you need ideas!
Ideas to do on New Years Eve if not going out the safest route to go!
1. Do a 1,000 piece puzzle.
2. Start binging a new TV show.
3. Host or go to a game night with less than 10 or better Zume it.
4. Make and then listen to a playlist of all of your favorite songs.
5. Or just do that thing where you play a song just before midnight, so that the best part plays right at 12 a.m. on Jan. 1.
6. Get Chinese or whatever takeout you want and watch Planet Earth 2 or another documentary or whatever you want to watch.
7. Take a nice, long bath with some salts or bubbles by yourself or with your significant other.
8. Although, if you want to start or read a book, now’s also a good time to do it. Don’t forget your favorite snack and drink as well.
9. Write letters to your friends and or family.
10. Treat it like you would the the last day of any other month, and do…whatever but be safe for you and others.
If you choose to take the safest route and celebrate solo or only with your own household, Good Housekeeping has loads of fun alternatives, such as making a New Year’s Brunch, decorating your space, scrapbooking your favorite memories from 2020, or getting dressed up as if you’re going to a party. Oprah Magazine suggests experimenting with fun cocktails, hosting a dinner party via Zoom, making a thoughtful resolutions list, or having a solo photoshoot with a DIY festive backdrop.
If all else fails, pour yourself a glass of champagne and watch a livestream of the ball dropping. We’re starting a brand new year here, and we want to ring it in with pride and positivity — not regrets.
In the end, we’d much rather have you nurse a hangover than a pandemic-level virus restarting (this is the flu and corona virus time again) or simply get sick before going back to work or not with bringing in the new year.
QUOTE FOR THE WEEKEND:
“New Years Eve is a great chance to celebrate the year gone by and the coming of a new one. However, these celebrations also come with great dangers and responsibilities. Here are a few tips to keep in mind as you make your New Years plans!
If you are celebrating New Years Eve away from your home or will be traveling at all, here are some ideas to keep you safe.
- Plan your travel options ahead of time, arranging for a designated driver, a hotel stay, shuttle/limo service, public transportation and extra “Plan B” options before your night out.
Host / Hostess providing a great party atmosphere, consider these tips to keep your guests safe.
- Make sure smoke alarms are working and have fresh batteries.
- Research numbers for local hospitals and authorities and have them ready in the case of an accident.
- Contact a local cab company to provide rides for your guests, or have a trusted designated driver ready to take guests home if necessary.
- Offer non-alcoholic drink options and have plenty of water available.
- Use differently colored cups for alcoholic and non-alcoholic beverages. Dump unattended cups so kids and pets do not consume them.
- Stop serving alcohol several hours before the party ends (and stick to it!).”
American Safety Council (» New Years Eve Safety Tips)