“Multiple sclerosis (MS) is a long-lasting (chronic) disease of the central nervous system. It is thought to be an autoimmune disorder, a condition in which the body attacks itself by mistake. MS is an unpredictable disease that affects people differently. Some people with MS may have only mild symptoms. Others may lose their ability to see clearly, write, speak, or walk when communication between the brain and other parts of the body becomes disrupted.”
QUOTE FOR MONDAY:
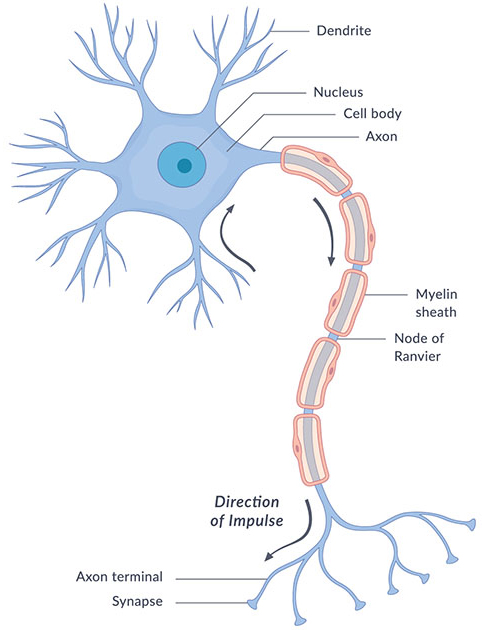
“The spinal cord is a long, tube-like band of tissue. It connects your brain to your lower back. Your spinal cord carries nerve signals from your brain to your body and vice versa. These nerve signals help you feel sensations and move your body. Any damage to your spinal cord can affect your movement or function. In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause permanent damage or deterioration of the nerves.”
MAYO CLINIC
The Nervous System Makeup in the human body!
The nervous system transmits signals between the brain and the rest of the body, including internal organs. In this way, the nervous system’s activity controls the ability to move, breathe, see, think, and more.
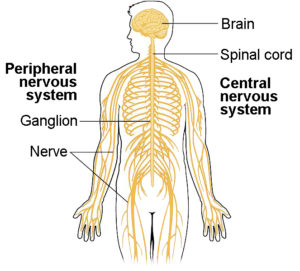
The nervous system is a complex, sophisticated system that regulates and coordinates body activities. It is made up of two major divisions or has 2 main parts, including the following:
1-CNS (Central Nervous System) and 2-PNS (Peripheral Nervous System)
- 1-Central nervous system. This consists of the brain and spinal cord. The central nervous system (defined as the brain and spinal cord) is usually considered to have seven basic parts: the spinal cord, the medulla, the pons, the cerebellum, the midbrain, the diencephalon, and the cerebral hemispheres
SUBDIVISION OF THE CENTRAL NERVOUS SYSTEM; CRANIAL NERVES:
Table 1.1The Cranial Nerves and Their Primary Functions
| Cranial nerve | Name | Sensory and/or motor | Major function | Location of cells whose axons form the nerve | Clinical test of function |
|---|---|---|---|---|---|
| I | Olfactory nerve | Sensory | Sense of smell | Nasal epithelium | Test sense of smell with standard odor |
| II | Optic nerve | Sensory | Vision | Retina | Measure acuity and integrity of visual field |
| III | Oculomotor nerve | Motor | Eye movements; papillary constriction and accommodation; muscles of eyelid. | Oculomotor nucleus in midbrain; Edinger-Westphal nucleus in midbrain | Test eye movements (patient can’t look up, down, or medially if nerve involved); look for ptosis, pupillary dilation |
| IV | Trigeminal nerve | Motor | Eye movements | Trochlear nucleus in midbrain | Can’t look downward when eye abducted |
| V | Trochlear nerve | Sensory and motor | Somatic sensation from face, mouth, cornea; muscles of mastication | Trigeminal motor nucleus in pons; trigeminal sensory ganglion (the gasserian ganglion) | Test sensation on face; palpate masseter muscles and temporal muscle |
| VI | Abducens nerve | Motor | Eye movements | Abducens nucleus in midbrain | Can’t look laterally |
| VII | Facial nerve | Sensory and motor | Controls the muscles of facial expression; taste from anterior tongue; lacrimal and salivary glands | Facial motor nucleus; superior salivatory nuclei in pons; trigeminal (gasserian) ganglion | Test facial expression plus taste on anterior tongue |
| VIII | Auditory/vestibular nerve | Sensory | Hearing;sense of balance | Spiral ganglion; vestibular (Scarpa’s) ganglion | Test audition with tuning fork; vestibular function with caloric test |
| IX | Glossopharyngeal nerve | Sensory and motor | Sensation from pharynx; taste from posterior tongue; carotid baroreceptors | Nucleus ambiguus; inferior salivatory | Test swallowing; pharyngeal gag reflex |
| X | Vague nerve | Sensory and motor | Autonomic functions of gut; sensation from pharynx; muscles of vocal cords; swallowing | Dorsal motor nucleus of vagus; vagal nerve ganglion | Test above plus hoarseness |
| XI | Accessory nerve | Motor | Shoulder and neck muscles | Spinal accessory nucleus; nucleus ambiguus; intermediolateral column of spinal cord | Test sternocleidomastoid and trapezius muscles |
| XII | Hypoglossal nerve | Motor | Movements of tongue | Hypoglossal nucleus of medulla | Test deviation of tongue during protrusion (points to side of lesion) |
- 2-Peripheral nervous system. This consists of all other neural elements, including the peripheral nerves and the autonomic nerves. This makes up a large division of the enteric nervous system which we will get into later. Also your peripheral nervous system contains your:
- Somatic nervous system, which guides your voluntary movements. The somatic nervous system is a component of the peripheral nervous system associated with the voluntary control of the body movements via the use of skeletal muscles.
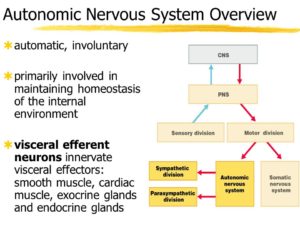
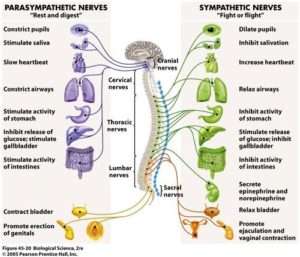
- Autonomic nervous system, which controls the activities you do without thinking about them; involuntary control (ex. Breathing). Autonomic Nervous System further breaks down into
.
3-The enteric nervous system (ENS) is a large division of the peripheral nervous system (PNS) that can control gastrointestinal behaviour independently of central nervous system (CNS) input. Mammalian neurons are located in either the CNS (brain and spinal cord) or PNS (cells with soma outside the brain and spinal cord).
The enteric nervous system (ENS) is a web of sensory neurons, motor neurons, and interneurons embedded in the wall of the gastrointesinal system, stretching from the lower third of the esophagus right through to the rectum.
The enteric nervous system (ENS) is known as the “second brain” or the brain in the gut because it can operate independently of the brain and spinal cord, the central nervous system (CNS). It has also been called the “first brain” based on evidence suggesting that the ENS evolved before the CNS.
So in review the makeup of the Autonomic Nervous System = Parasympathetic, Sympathetic & Enteric Nervous Systems. Further subdividing down to the somatic and visceral nervous systems.
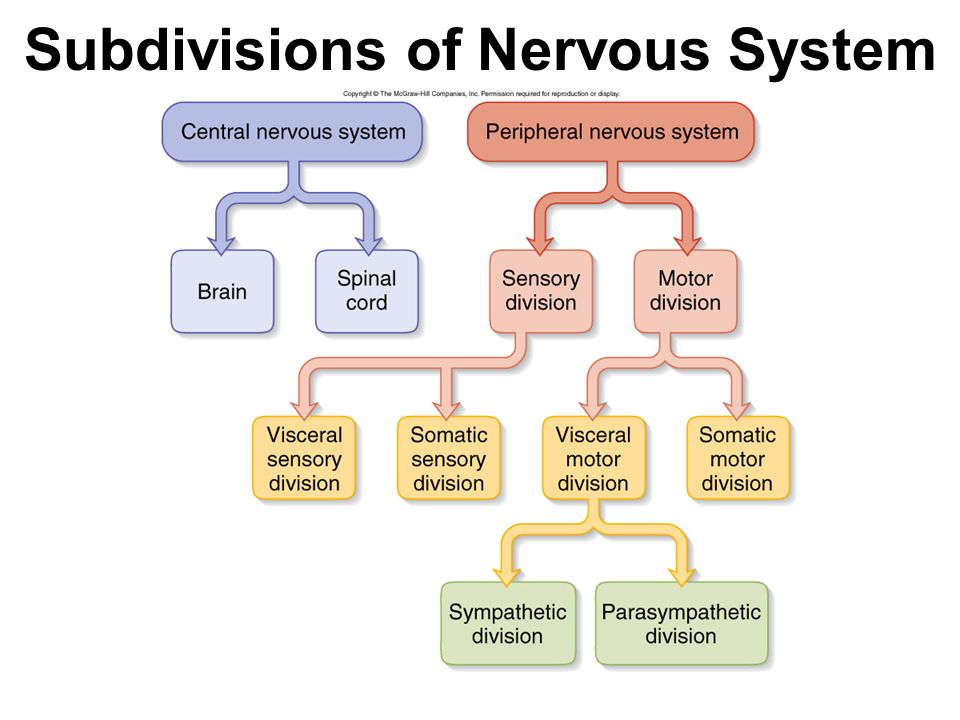
Somatic sensory input comes from the receptors of the eyes, ears, nose, tongue, and skin. These organs transmit information we associate with the five senses; making up the somatic nervous system in the peripheral nervous system.
Visceral sensory input comes from (surprise!) the viscera, or internal organs; making up the visceral nervous system in the peripheral nervous system.
QUOTE FOR THE WEEKEND:
“.Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system).”
MAYO CLINIC
How does MS-Multiple Sclerosis affect these areas, and what are some of the issues MS causes is what we cover next week due to March is MS month!
QUOTE FOR FRIDAY:
“Invasive Meningococcal Disease (IMD) is caused by meningococcal bacteria, and is almost always meningitis or septicaemia (also known as sepsis), less frequently pneumonia or infection in other parts of the body. Although it has been widely known that meningitis and septicaemia can cause death swiftly, recent analysis from a team of researchers at PHE quantified precisely how swiftly the disease acts in different age groups. The research helps highlight the importance of rapid treatment. This new study shows that for most of those who die of this leading cause of meningitis, the disease comes on suddenly and advances rapidly, with a very limited time window to administer life-saving treatment, underlining the importance of prevention=Vaccine.”
Centers for Disease Control and Prevention (CDC)
Part 2 Meningococcal Meningitis
Your risk for meningococcal meningitis increases if you are exposed to the bacterium that causes it. Your risk also increases if you’ve had a recent upper respiratory infection. Babies, children, teens, and the elderly are at greatest risk.
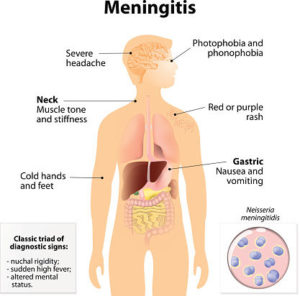
Signs & symptoms of meningococcal meningitis may vary from case to case. The more common S/S:
- General poor feeling
- Sudden high fever
- Severe, persistent headache
- Neck stiffness
- Nausea or vomiting
- Discomfort in bright lights
- Drowsiness or difficulty awakening
- Joint pain
- Confusion or other mental changes
A reddish or purple skin rash (known as petechiae)!!!!! This is a very important sign to watch for. If it does not turn white when you press on it with a glove the rash may be a sign of bacteremia, or a bacterial infection in the bloodstream. This is a medical emergency.
- Tense or bulging soft spot (in babies)
- High-pitched or moaning cry (in babies)
- Stiff, jerky movements or floppiness (in babies or toddlers)
- Irritability
- Fast breathing
- Lethargy or excessive sleepiness
- Blotchy skin, turning pale or blue
- Shivering, or cold hands and feet
- Seizure
Meningococcal meningitis can cause death or serious complications, such as brain damage, paralysis, gangrene, or deafness. To prevent these problems, it’s important to act quickly. Do not wait. Seek immediate medical attention. Go to an emergency room or call 911 if:
- You notice symptoms of meningococcal meningitis.
- Symptoms do not improve with treatment.
- You think you have been exposed to meningococcal meningitis.
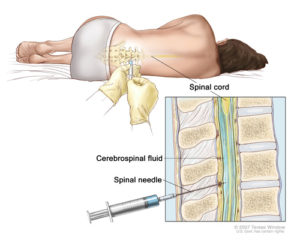
How its diagnosed:
Tests can confirm a diagnosis of meningococcal meningitis; Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to those of other illnesses. If a doctor suspects meningococcal disease, they will collect samples of blood or cerebrospinal fluid (fluid near the spinal cord). Doctors then send the samples to a laboratory for testing.
Treatments:
The doctor may start antibiotics, such as penicillin or ceftriaxone, by an IV, or intravenous line. You or your child may also need other medication to treat problems related to increased spinal fluid pressure. Doctors sometimes prescribe steroids for antiinflammatory effect or the spinal cord. Penicillin is the drug of choice for the treatment of meningococcal meningitis and septicemia. Chemoprophylactic antimicrobials most commonly used to eradicate meningococci include rifampin, quinolones (eg, ciprofloxacin), ceftriaxone. Also included in this class are minocycline and spiramycin.
Meningococcal meningitis is a serious disease — even with treatment. That’s why prevention is a far better approach. The meningococcal vaccine can prevent meningitis infection. In the U.S., three types of meningococcal vaccines are used that are:
- Meningococcal conjugate vaccine (MCV4) — is approved for people ages 9 months to 55.
- Meningococcal polysaccharide vaccine (MPSV4) — This vaccine was approved in the 1970s and protects against most forms of meningococcal disease. This vaccine used is for people as young as 9 months and older than age 55.
- Serogroup B Meningococcal B (MenB) – Both are licensed for ages 10-24 but can be used in older patients also.
QUOTE FOR THURSDAY:
“Meningococcal meningitis is a rare but serious bacterial infection. Meningococcal, serious illness caused by a bacteria (Neisseria meningitidis). It can cause meningitis, which is an infection of the brain and spinal cord, and it can also cause blood infections. It causes the membranes that cover the brain and spinal cord to become inflamed. Each year, approximately 1,000 people in the U.S. get meningococcal disease, which includes meningitis and septicemia (blood infection).
Meningococcal meningitis can be fatal or cause great harm without prompt treatment; as many as one out of five people who contract the infection have serious complications. According to the Centers for Disease Control, even with antibiotics, 10 to 15% of those infected will die and about 1 in 5 of those who survive are left with long-term disabilities that include deafness, brain damage, neurological problems, and even loss of a limb. There is a way to prevent it.” (which will be discussed tomorrow on our blog).
NMA – National Meningitis Association
QUOTE FOR WEDNESDAY:
“A brain injury is any occurrence that causes damage to your brain. The scope of what qualifies as a brain injury is fairly large. Brain injury can be anything from a mild concussion to traumatic brain injury, also known as craniocerebral trauma. Mild traumatic brain injury may affect your brain cells temporarily. More-serious traumatic brain injury can result in bruising, torn tissues, bleeding and other physical damage to the brain. These injuries can result in long-term complications or death (like bullet, shattered piece of skull, .
Not all brain injury results in TBI. In fact, some low-grade concussions may heal just fine on their own but any head hit or injury have checked by MD or ER.”
MAYO CLINIC
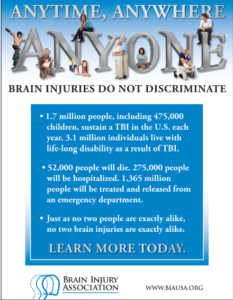
Part II National Brain Injury Awareness Month!
What are the causes?
Common causes include falls, car or motorcycle crashes, vehicular accidents involving pedestrians, athletics, and assaults with or without a weapon.
Who is affected?
Approximately 1.5 to 2 million adults and children suffer a traumatic brain injury (TBI) each year in the United States. Most people who experience a head injury, about 1.1 million, will have a mild injury that does not require an admission to the hospital. Another 235,000 individuals will be hospitalized with a moderate to severe head injury, and approximately 50,000 will die.
How is a diagnosis made?
When a person is brought to the emergency room with a head injury, doctors will learn as much as possible about his or her symptoms and how the injury occurred. The person’s condition is assessed quickly to determine the extent of injury.
The Glasgow Coma Score (GCS) is a 15-point test used to grade a patient’s level of consciousness. Doctors assess the patient’s ability to 1) open his or her eyes, 2) ability to respond appropriately to orientation questions, (“What is your name? What is the date today?”), and 3) ability to follow commands (“Hold up two fingers, or give a thumbs up”). If unconscious or unable to follow commands, his or her response to painful stimulation is checked. A number is taken from each category and added together to get the total GCS score. The score ranges from 3 to 15 and helps doctors classify an injury as mild, moderate, or severe. Mild TBI has a score of 13-15. Moderate TBI has a score of 9-12, and severe TBI has a score of 8 and below.
Diagnostic imaging tests will be performed:

Figure 3. CT scan shows a blood clot (hematoma) collecting under the bone (red arrows) and displacing brain (yellow arrow) to the other side of the skull.
- Computed Tomography (CT) is a noninvasive X-ray that provides detailed images of anatomical structures within the brain. A CT scan of the head is taken at the time of injury to quickly identify fractures, bleeding in the brain, blood clots (hematomas) and the extent of injury (Fig. 3). CT scans are used throughout recovery to evaluate the evolution of the injury and to help guide decision-making about the patient’s care.
- Magnetic Resonance Imaging (MRI) is a noninvasive test that uses a magnetic field and radiofrequency waves to give a detailed view of the soft tissues of the brain. A dye (contrast agent) may be injected into the patient’s bloodstream. MRI can detect subtle changes in the brain that cannot be seen on a CT scan.
- Magnetic Resonance Spectroscopy (MRS) gives information about the metabolism of the brain. The numbers generated from this scan provide a general prognosis about the patient’s ability to recover from the injury.
What treatments are available?
Mild TBI usually requires rest and medication to relieve headache. Moderate to severe TBI require intensive care in a hospital. Bleeding and swelling in the brain can become an emergency that requires surgery. However, there are times when a patient does not require surgery and can be safely monitored by nurses and physicians in the neuroscience intensive care unit (NSICU).
The goals of treatment are to resuscitate and support the critically ill patient, minimize secondary brain injury and complications, and facilitate the patient’s transition to a recovery environment. Despite significant research, doctors only have measures to control brain swelling, but do not have a way to eliminate swelling from occurring.
Neurocritical care
Neurocritical care is the intensive care of patients who have suffered a life-threatening brain injury. Many patients with severe TBI are comatose or paralyzed; they also may have suffered injuries in other parts of the body. Their care is overseen by a neurointensivist, a specialty-trained physician who coordinates the patient’s complex neurological and medical care. Patients are monitored and awakened every hour for nursing assessments of their mental status or brain function.
Figure 4. In the NSICU, the patient is connected to numerous machines, tubes, and monitors. The monitoring equipment provides information about body functions and helps guide care. Some equipment may take over certain functions, such as breathing, nutrition, and urination, until the patient’s body is able to do these things on its own.
Seeing a patient who has suffered a severe TBI can be shocking. It is possible that your loved one’s appearance will be altered because of facial injury and equipment that is used for monitoring. Numerous tubes, lines, and equipment may be used to closely monitor his or her heart rate, blood pressure, and other critical body functions. (Fig. 4)

Figure 5. A brain oxygen and cerebral blood flow monitor is inserted into the brain tissue and secured to the skull with a bolt. A catheter is inserted into the ventricle of the brain to monitor intracranial pressure (ICP). If pressure is too high, the CSF fluid can be drained from the ventricles.
- Intracranial pressure (ICP) monitor. A catheter is placed through a small hole in the skull and positioned inside the ventricle (fluid-filled area deep within the brain) to measure pressure inside the head (Fig. 5). The ICP monitor allows the NSICU team to intervene quickly if the pressure becomes too high. Typical intracranial pressure is less than 20 mmHg. However, there are times when a higher number is safe and acceptable.
- Brain oxygen monitor (Licox). A catheter is placed through a small hole in the skull and positioned within the brain tissue. The Licox measures the oxygen level and temperature within the brain. Adjustments in the amount of oxygen given to the patient are often made to maximize the brain’s oxygen level. A cerebral blood flow monitor, called a Hemedex, is a newer monitor that is placed with the Licox and helps the NSICU team evaluate blood flow through the brain.
- Ventilator. Some patients may require a ventilator, a machine that helps them breathe. The ventilator is connected to the patient by the endotracheal tube, or ET tube. The tube is placed into the patient’s mouth and down into the trachea, or windpipe. The tube allows the machine to push air into and out of the lungs, thereby helping the patient breathe.
- Feeding tube. When patients are on a ventilator or have a decreased level of alertness, they may not be able to eat or get sufficient nutrition to meet their needs. A nasal-gastric feeding tube may be inserted through the patient’s nose and passed down the throat into the stomach. It delivers liquid nutrition as well as any medication that is required.
- Seizures and EEG monitoring. A seizure is an abnormal electrical discharge from the brain. Approximately 24% of patients who suffer a TBI will have a seizure that is undetected unless they are monitored by an electroencephalogram (EEG). Seizures that are not visible to the human eye are referred to as non-convulsive seizures. Because these seizures are serious, all patients with a severe TBI are monitored with continuous EEG for 24 to 72 hours after injury.
Medication
- Sedation and pain. After a head injury it may be necessary to keep the patient sedated with medications. These medications can be turned off quickly in order to awaken the patient and check their mental status. Because patients often have other injuries, pain medication is given to keep them comfortable.
- Controlling intracranial pressure. Hypertonic saline is a medication used to control pressure within the brain. It works by drawing the extra water out of the brain cells into the blood vessels and allowing the kidneys to filter it out of the blood.
- Preventing seizures. Patients who’ve had a moderate to severe traumatic brain injury are at higher risk of having seizures during the first week after their injury. Patients are given an anti-seizure medication (levetiracetam or phenytoin) to prevent seizures from occurring.
- Preventing infection. Although every attempt is made to prevent infection, the risk is always present. Any device placed within the patient has the potential to introduce a microbe. If an infection is suspected, a test will be sent to a laboratory for analysis. If an infection is present, it will be treated with antibiotics.
Surgery
Surgery is sometimes necessary to repair skull fractures, repair bleeding vessels, or remove large blood clots (hematomas). It is also performed to relieve extremely high intracranial pressure.
- Craniotomy involves cutting a hole in the skull to remove a bone flap so that the surgeon can access the brain. The surgeon then repairs the damage (e.g., skull fracture, bleeding vessel, remove large blood clots). The bone flap is replaced in its normal position and secured to the skull with plates and screws.

Figure 6. A large decompressive craniectomy is removed and the dura is opened to allow the brain to expand. Blood clots are removed and bleeding vessels are repaired. The bone flap is frozen and replaced about 6 weeks later.
- Decompressive craniectomy involves removing a large section of bone so that the brain can swell and expand. This is typically performed when extremely high intracranial pressure becomes life threatening. At that time the patient is taken to the operating room where a large portion of the skull is removed to give the brain more room to swell (Fig. 6). A special biologic tissue is placed on top of the exposed brain and the skin is closed. The bone flap is stored in a freezer. One to 3 months after the swelling has resolved and the patient has stabilized from the injury, the bone flap is replaced in another surgery, called cranioplasty.
Other surgical procedures may be performed to aid in the patient’s recovery:
- Tracheotomy involves making a small incision in the neck to insert the breathing tube directly into the windpipe. The ventilator will then be connected to this new location on the neck and the old tube is removed from the mouth.
- Percutaneous Endoscopic Gastrostomy Tube (PEG) is a feeding tube inserted directly into the stomach through the abdominal wall. A small camera is placed down the patient’s throat into the stomach to aid with the procedure and to ensure correct placement of the PEG tube (see Surgical Procedures for Accelerated Recovery).
Clinical trials
Clinical trials are research studies in which new treatments—drugs, diagnostics, procedures, and other therapies—are tested in people to see if they are safe and effective. Research is always being conducted to improve the standard of medical care. Information about current clinical trials, including eligibility, protocol, and locations, are found on the Web. Studies can be sponsored by the National Institutes of Health (see clinicaltrials.gov) as well as private industry and pharmaceutical companies (see www.centerwatch.com).
Recovery & prevention
The recovery process varies depending on the severity of the injury, but typically progresses through stages: coma, confusion / amnesia, and recovery.
- When a patient is in a coma, his or her eyes are closed and they show minimal reaction when spoken to or stimulated. Movements that may be seen at this time are basic reflexes or automatic responses to a stimulus. The brain wave activity in a comatose person is very different from that of a sleeping person.
- When a patient begins to awaken, the first natural response is that of bodily protection. Patients at this stage will move away from any stimulus or tend to pull at items attached to them in an attempt to remove anything that is uncomfortable or irritating. His or her eyes may be open more often, but they may not be aware of their behavior or be able to interact in a meaningful way. It is common for a patient to respond to each stimulus (hearing, seeing, or touching) in the same way. Responses may include increased rate of breathing, moaning, moving, sweating, or a rise in blood pressure.
- As the patient continues to wake up, their interactions may become more purposeful. They may look at a person and follow them around the room with their eyes, or follow simple commands such as “Hold up your thumb.” Patients tend to be confused and may have inappropriate or agitated behaviors.
Not all head injuries are the same. Patients recover at different rates and to varying degrees. It is difficult to determine at what point a patient will start understanding and interacting with their caregivers or family in a meaningful way. It is important to have patience; recovery from a brain injury can take weeks, months, or even years.
The Family’s Role
Many family members express feelings of helplessness when their loved one is in the NSICU. You are not alone. Please take care of yourself and use your energy wisely.
Visiting hours are limited in the NSICU. Too much stimulation can agitate the patient and raise his or her blood pressure. You can most effectively convey your concern by sitting quietly and holding your loved one’s hand. Be aware that the patient, though silent, may hear anything you say. Never speak as if the patient were not there.
As patients recover, they need help understanding what has happened to them during this “lost period of time.” Keep in mind that the recovery of consciousness is a gradual process – not just a matter of waking up. Progress is usually tracked in three areas: movement, thinking, and interacting. You can help by keeping a diary of their progress. Family photos may help with regaining memory.
Rehabilitation
Most patients are discharged from the hospital when their condition has stabilized and they no longer require intensive care. A social worker will work closely with the family as preparations are made for a return home or for transfer to a long-term care or rehabilitation center.
- A long-term acute care (LTAC) facility is a place for patients who have stabilized from their initial injury but who still require a ventilator or frequent nursing care. Many patients are discharged to an LTAC to continue being weaned from the ventilator. Once off the ventilator, they can be moved to a rehabilitation or skilled nursing facility.
- A rehabilitation facility is a place for patients who do not require a ventilator but who still require help with basic daily activities. Physical and occupational therapists work with patients to help them achieve their maximum potential for recovery. Rehab facilities are either Acute Inpatient Rehab that require patients to participate in 3 hours or more of rehab a day or a Skilled Nursing Facility (SNF) that provide 1-3 hours of rehab a day depending on what the patient can tolerate.
Recovering from a brain injury relies on the brain’s plasticity—the ability for undamaged areas of the brain to take over functions of the damaged areas. It also relies on regeneration and repair of nerve cells. And most importantly, on the patient’s hard work to relearn and compensate for lost abilities.
- A physical therapist helps patients rebuild and maintain strength, balance, and coordination. They can work with the patient in any facility.
- An occupational therapist helps patients to perform activities of daily living, such as dressing, feeding, bathing, toileting, and transferring themselves from one place to another. They also provide adaptive equipment if a patient has difficultly performing a task.
- A speech therapist helps patients by monitoring their ability to safely swallow food and helping with communication and cognition.
- A neuropsychologist helps patients relearn cognitive functions and develop compensation skills to cope with memory, thinking, and emotional needs.
Prevention
Tips to reduce the risk for a head injury:
- Always wear your helmet when riding a bicycle, motorcycle, skateboard, or all-terrain vehicle.
- Never drive under the influence of alcohol or drugs.
- Always wear your seat belt and ensure that children are secured in the appropriate child safety seats.
- Avoid falls in the home by keeping unsecured items off the floor, installing safety features such as non-slip mats in the bathtub, handrails on stairways, and keeping items off of stairs.
- Avoid falls by exercising to increase strength, balance, and coordination.
- Store firearms in a locked cabinet with bullets in a separate location.
- Wear protective headgear while playing sports.
Reference for Part I and Part II: Mayfield Brain & Spine at 513-221-1100.
QUOTE FOR TUESDAY:
“National Brain Injury Awareness Month! Every year the Brain Injury Association of America (BIAA) proudly leads Americans throughout Brain Injury Awareness Month. The theme for this year is #ChangeYourMind. And its goal is to:
- Help de-stigmatize brain injury in the community,
- Share the stories of those who are living with brain injuries, and those that care for them,
- And spread awareness of the ways people living with brain injuries can receive support.”
BrainForest (brainforest.com)