1. Proper eating, sleeping, exercising, and enjoying hobbies can often take a back seat to other priorities during the holidays. This again is setting the stage for disappointment as lack of self-care erodes the ability to cope with the increased stressors of the holidays. A growing body of evidence stresses the importance of this practice, and the number of effective interventions continues to expand (Jaarsma et al., 2020). Davis (2018) and other experts are widely available online for those who would like to learn more.
2.Be realistic. The holidays don’t have to be perfect or just like last year. As families change and grow, traditions and rituals often change as well. Choose a few to hold on to, and be open to creating new ones. For example, if your adult children or other relatives can’t come to your home, find new ways to celebrate together, such as sharing pictures, emails or videos. Or meet virtually on a video call. Even though your holiday plans may look different this year, you can find ways to celebrate and be grateful for.
3.Reach out. If you feel lonely or isolated, seek out community, religious or other social events or communities. Many may have websites, online support groups, social media sites or virtual events. They can offer support and companionship.
If you’re feeling stress during the holidays, it also may help to talk to a friend or family member about your concerns. Try reaching out with a text, a call or a video chat.
Volunteering your time or doing something to help others also is a good way to lift your spirits and broaden your friendships.
4. Set aside differences. Try to accept family members and friends as they are, even if they don’t live up to all of your expectations. Set aside grievances until a more appropriate time for discussion. And be understanding if others get upset or distressed when something goes awry. Like our parents taught us at a gathering don’t talk about religion or politics, especially if you don’t know what they favor. This is more of a chance to make your day less stressful.
5. Say no if you have to and family and friends should would understand this especially after this covid-19 year. Some families would like less crowds at the party for health, which should come first. Less chance of the host or hostess becoming resentful they said yes and you could always zoom online with the family or friends you would normally see. Less stress as well.
6. Very important as well budget out what you plan to spend. Before you do your gift and food shopping, decide how much money you can afford to spend. Then stick to your budget. Don’t try to buy happiness with an avalanche of food and gifts.
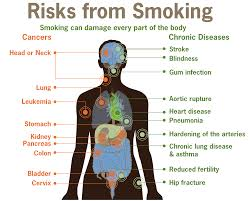
7. Lastly remember your health! Don’t let the holidays become a free-for-all. Overindulgence with foods and gifts only adds to your stress and guilt.