The Sun is by far the largest object in the solar system. It contains more than 99.8% of the total mass of the Solar System (Jupiter contains most of the rest).
It is often said that the Sun is an “ordinary” star. That’s true in the sense that there are many others similar to it. But there are many more smaller stars than larger ones; the Sun is in the top 10% by mass. The median size of stars in our galaxy is probably less than half the mass of the Sun. A process called fusion heats the Sun. Fusion happens in the core of the Sun. It is very hot there. In fact, the core’s average temperature is around 27,000,000 degrees Fahrenheit. The surface of the Sun is cool compared with the core, only 10,000 degrees Fahrenheit.
This fusion process not only heats the Sun, it makes the sunlight we see here on Earth. This sunlight travels the speed of light which is 186,282 miles per second or 299,792,458 meters per second. This means the light from the Sun takes 8.4 minutes to travel 93 million miles to Earth. If the world’s fastest land animal were to travel that same distance, it would take a cheetah over 151 years to reach the Earth running about 70 mph nonstop!
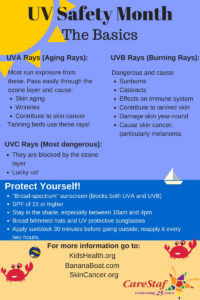
Ultraviolet radiation: Invisible rays that are part of the energy that comes from the sun. Ultraviolet radiation can burn the skin and cause skin cancer.
Ultraviolet radiation is made up of three types of rays — ultraviolet A, ultraviolet B, and ultraviolet C. Although ultraviolet C is the most dangerous type of ultraviolet light in terms of its potential to harm life on earth, it cannot penetrate earth’s protective ozone layer. Therefore, it poses no threat to human, animal or plant life on earth.
Ultraviolet A and ultraviolet B, on the other hand, do penetrate the ozone layer in attenuated form and reach the surface of the planet. Because ultraviolet A is weaker than ultraviolet B, scientists long blamed ultraviolet B as the sole culprit in causing skin cancer in persons with a history of sunburn and repeated overexposure to ultraviolet radiation. Recent research, however, has also implicated ultraviolet A as a possible cause of skin cancer.
Photosensitivity refers to various symptoms, diseases and conditions caused or aggravated by exposure to sunlight.
- A rash due to photosensitivity is a photodermatosis (plural photodermatoses).
- If the rash is eczematous, it is a photodermatitis.
- A chemical or drug that causes photosensitivity is a photosensitiser.
- A phototoxic reaction to a photosensitiser results in an exaggerated sunburn reaction and no immune reaction is involved.
- A photoallergic reaction to a photosensitiser results in photodermatitis and is due to delayed hypersensitivity reaction.
- A photoexacerbated condition describes a flare of an underlying skin disease on exposure to sunlight.
Photosensitivity is characterized into many groups:
- Polymorphic light eruption (PLE):
PLE generally affects adult females aged 20–40, although it sometimes affects children and males (25%). It is particularly common in places where sun exposure is uncommon, such as Northern Europe, where it is said to affect 10–20% of women holidaying in the Mediterranean area. It is less common in Australasia. It has also been reported to be relatively common at higher altitudes compared to sea level.
PLE can occur in all races and skin phototypes and may be more prevalent in skin of colour than in white skin. There is a genetic tendency to PLE, and it is sometimes associated with or confused with photosensitivity due to lupus erythematosus (which generally is more persistent than PLE).
Some patients experience PLE during phototherapy, which is used to treat skin conditions such as psoriasis and dermatitis.
There are three types of UV rays:
Ultraviolet A (UVA): UVA rays penetrate deep into the layers of the skin and lead to premature signs of aging, which include fine lines and wrinkles. It is important to note that the amount of UVA stays relatively consistent throughout the year, and exceeds the amount of UVB in both summer and winter. Even on a cloudy day, 80% of the sun’s UVA rays pass through the clouds and reach our skin and eyes. It’s also important to know that tanning beds work by emitting primarily UVA rays.
Ultraviolet B (UVB): UVB rays are the primary cause of sunburn, thickening of the skin, and several types of skin cancers – including melanoma. UVB rays penetrate the outermost layer of skin and cause damage to skin cells. UVB also can cause damage to eyes and the immune system.
Ultraviolet C (UVC): UVC is the strongest of the UV spectrum radiation. Fortunately, UVC rays do not reach the earth’s surface because it is blocked by the ozone layer of the atmosphere. The only way we can be exposed to UVC radiation is from an artifical source, such as a lamp or laser. UVC rays can cause severe skin burns and eye injuries even when exposed for only a few seconds. Since the penetration depth of UVC rays is very low, these injuries usually resolve within a week with virtually no risk of long-term health risks (skin cancer, cateracts, vision loss).
Causes:
Genetic factors may be important with many affected individuals reporting a family history of PLE. Native Americans have a hereditary form of PLE (actinic prurigo).
PLE is caused by a delayed hypersensitivity reaction to a compound in the skin that is altered by exposure to ultraviolet radiation (UVR). UVR leads to impaired T cell function and altered production of cytokines in affected individuals. There is a reduction in the normal UV-induced immune suppression in the skin. This has been suggested to be either due to oestrogen or deficiency of vitamin D.
The rash is usually provoked by UVA (in 90%). This means the rash can occur when the sunlight is coming through window glass, and that standard sunscreens may not prevent it. Occasionally, UVB and/or visible light provoke PLE.
PLE may be a rare occurrence in the individual concerned or may occur every time the skin is exposed to sunlight. In most affected individuals, it occurs each spring, provoked by several hours outside on a sunny day. If further sun exposure is avoided, the rash settles in a few days and is gone without a trace within a couple of weeks. It can recur next time the sun shines on the skin. However, if the affected area is exposed to more sun before it has cleared up, the condition tends to get more severe and extensive with longer to heal.
Stay tune tomorrow for part II on Ultralight rays from the Sun to Sunburn and Types of photosensitivity for some!