
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer, and then can spread to other areas of the body.
Gastrointestinal stromal tumors (GISTs) are not common, and the exact number of people diagnosed with these tumors each year is not known. Until the late 1990s, not much was known about these tumors (and doctors didn’t have good ways of identifying them with lab tests), so many of them ended up being classified as other kinds of cancers.
Current estimates for the total number of GIST cases diagnosed each year in the United States range from about 4,000 to about 6,000.
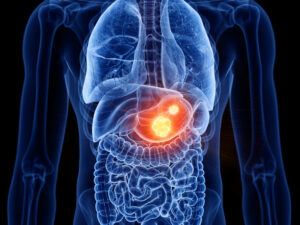
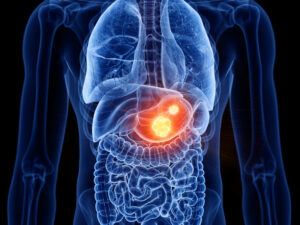
A gastrointestinal stromal tumor (GIST) is a type of cancer that begins in the digestive system. GISTs happen most often in the stomach and small intestine.
A GIST is a growth of cells that’s thought to form from a special type of nerve cells. These special nerve cells are in the walls of the digestive organs. They play a part in the process that moves food through the body.
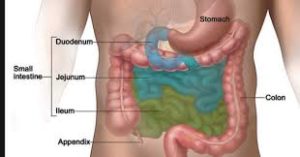
The GI tract processes food for energy and rids the body of solid waste. After food is chewed and swallowed, it goes through the esophagus, a tube that carries food down the throat and chest to the stomach. The esophagus joins the stomach just beneath the diaphragm (the thin band of muscle below the lungs).
The stomach is a sac-like organ that helps the digestive process by mixing the food with gastric juices. The food and gastric juices are then emptied into the small intestine. The small intestine, which is about 20 feet long, continues breaking down the food and absorbs most of the nutrients into the bloodstream.
The small intestine joins the large intestine, the first part of which is the colon, a muscular tube about 5 feet long. The colon absorbs water and mineral nutrients from the remaining food matter. The waste left after this process (stool) goes into the rectum, where it is stored until it passes out of the body through the anus.
Gastrointestinal stromal tumors (GISTs) are uncommon cancers that start in special cells in the wall of the gastrointestinal (GI) tract, also known as the digestive tract. To understand GISTs, it helps to know something about the structure and function of the GI tract.
Gastrointestinal stromal tumors (GISTs) start in very early forms of special cells in the wall of the GI tract called the interstitial cells of Cajal (ICCs). ICCs are sometimes called the “pacemakers” of the GI tract because they signal the muscles in the GI tract to contract to move food and liquid along.
More than half of GISTs start in the stomach. Most of the others start in the small intestine, but GISTs can start anywhere along the GI tract. A small number of GISTs start outside the GI tract in nearby areas such as the omentum (an apron-like layer of fatty tissue that hangs over the organs in the abdomen) or the peritoneum (the thin lining over the organs and walls inside the abdomen).
Some GISTs seem to be much more likely than others to grow into other areas or spread to other parts of the body. Doctors look at certain factors to help tell whether a GIST is likely to grow and spread quickly, such as:
- The size of the tumor
- Where it’s located in the GI tract
- How fast the tumor cells are dividing (its mitotic rate, described in Tests for Gastrointestinal Stromal Tumors)
Small GISTs may cause no symptoms, and they may grow so slowly that they don’t cause problems at first. As a GIST grows, it can cause signs and symptoms. They might include:
- Abdominal pain
- A growth you can feel in your abdomen
- Fatigue
- Nausea
- Vomiting
- Cramping pain in the abdomen after eating
- Not feeling hungry when you would expect to
- Feeling full if you eat only a small amount of food
- Dark-colored stools caused by bleeding in the digestive system
GISTs can happen in people at any age, but they are most common in adults and very rare in children. The cause of most GISTs isn’t known. A small number are caused by genes passed from parents to children.
GISTs are not the same as other, more common types of GI tract cancers that develop from other types of cells.
Cancers can occur anywhere in the GI tract − from the esophagus to the anus. Most cancers that start in the GI tract, including most esophagus cancers, stomach cancers, and colon and rectum cancers, start in the gland cells that line almost all of the GI tract. The cancers that develop in these cells are called adenocarcinomas.
Cancers can also start in squamous cells, which are flat cells that line some parts of the GI tract, like the upper part of the esophagus and the end of the anus. Cancers starting in these cells are called squamous cell carcinomas.
The GI tract also has neuroendocrine cells. These cells have some features in common with nerve cells but also have other features in common with hormone-producing (endocrine) cells. Cancers that develop from these cells are called neuroendocrine tumors (NETs). These cancers are rare in the GI tract. Carcinoid tumors are an example of a neuroendocrine tumor found in the GI tract.
Other rare types of cancer in the GI tract include different types of soft tissue sarcomas, such as:
- Leiomyosarcomas: cancers of smooth muscle cells
- Angiosarcomas: cancers of blood vessel cells
- Malignant peripheral nerve sheath tumors (MPNSTs): cancers of cells that support and protect nerves
GISTs are different from these other types of GI tract cancers. They start in different types of cells, need different types of treatment, and have a different prognosis (outlook). This is why doctors need to figure out whether a person with a tumor in the GI tract has a GIST, some other type of cancer, or a non-cancerous condition.
How it is diagnosed:
First you M.D. will do a physical exam.
They may also do the following tests:
- Upper endoscopy.
- Computed tomography (CT) scan.
- Positron emission tomography (PET).
- Biopsy to obtain tissue for a pathologist to examine under a microscope.
Treatment:
The most common treatment is surgery to remove the tumors.
Survival:
Survival rates vary depending on tumor size and activity at the time of diagnosis, your overall health and the tumor’s response to treatment. Overall, data from the U.S. National Cancer Institute (NCI) show that 85% of people with GIST were alive five years after diagnosis.