-STRESS REDUCTION
Stress is defined as feeling tense on the inside due to pressures from the outside. Most of us have many of these pressures, and some handle them better than others. Since stress makes the heart work harder, try to find ways to relieve the pressure you felt when stressed.
One way of coping with stress is to deal with your feelings. You may feel depressed, angry or anxious because you have high blood pressure. These feelings are normal. It may help to talk about how you feel with your family and friends. When you accept that you have high B/P, you can put your efforts into living a more productive, good life with dealing with the hypertension.
Many people find yoga, meditation and prescribed exercise helpful. Always check with your doctor before starting an exercise program to make sure you get clearance of what is safe for you by your primary doctor or cardiologist.
-Eat less SODIUM
Sodium is an important substance. It helps your body balance the level of fluid inside and outside of the cells. To keep up this balance, the body needs about 2000mg of sodium a day or less. Yet most of us eat 3000 to 6000mg of sodium each day.
Most people with high b/p are asked to eat less sodium. Sodium attracts water and makes the body hold fluid. To pump the added fluid the heart works harder. Also sodium in the body causes the arteries to vasocontrict increasing pressure in the vessels causing the pressure to rise.
Most people with high b/p are asked to eat less sodium at 2000mg or less a day and this is to prevent water retention and vasoconstriction in which both actions increase the blood pressure. Follow your doctor’s advice about your sodium intake.
Many prepared foods and spices are high in sodium. But, the most common source of sodium is table salt. Table salt is 40% sodium and 60% chloride. One teaspoon of table salt contains 2000mg of sodium.
HINTS TO LOWER YOUR SODIUM IN YOUR DIET:
-Season foods with fresh or dried herbs, vegetables, fruits or no-salt seasonings.
-Do not cook with salt or add salt to foods after they are on the table.
-Make your own breads, rolls, sauces, salad dressings, vegetable dishes and desserts when you can.
-Stay away from fast foods. They are almost all high in salt.
-Eat fresh, frozen or canned, unsalted vegetables. These have less sodium than most processed foods. Read the labels and if they don’t have a label DON’T EAT IT. Read the labels and eat the portioned size it says to for 1 portion with keeping a diary of what you ate with adding the sodium and when it reached 2000mg no more food that day with salt in it unless the doctor prescribes less.
-Buy water packed tuna and salmon. Break it up into a bowl of cold water, and let stand for 3 minutes. Rinse, drain and squeeze out water.
-Don’t buy convenience foods such as prepared or skillet dinners, deli foods, cold cuts, hot dogs, frozen entrees or canned soups. These have lots of salt. Be picky on what you eat.
-Again, read all labels for salt, sodium or sodium products (such as sodium benzoate, MSG). Ingredients are listed in the order of amount used. A low sodium label means 140mg of less per serving. Try to buy products labeled low sodium/serving. Do not eat products that have more sodium than this per serving.
-AHA states, “If you drink, limit your alcohol consumption to no more than two drinks per day for men and no more than one drink per day for women. A drink is one 12 oz. beer, 4 oz. of wine, 1.5 oz. of 80-proof spirits or 1 oz. of 100-proof spirits.
I’ve read that red wine is heart healthy — can I drink as much as I’d like?
Unfortunately, red wine as a miracle drink for heart health is a myth. The linkage reported in many of these studies may be due to other lifestyle factors rather than alcohol. Like any other dietary or lifestyle choice, it’s a matter of moderation and disciplining yourself to have mostly anything in life in moderation; especially when in comes to controlling your blood pressure.
If you need help–
If cutting back on alcohol is hard for you to do on your own, ask your healthcare provider about getting help.”
The AHA also states, “Lifestyle plays an important role in treating your high blood pressure. If you successfully control your blood pressure with a healthy lifestyle, you might avoid, delay or reduce the need for medication.
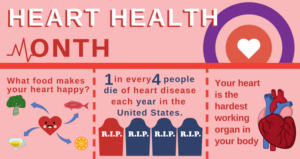
High blood pressure is a “silent killer”
You may not feel that anything is wrong, but high blood pressure could be quietly causing damage that can threaten your health. The best prevention is knowing your numbers and making changes that matter in order to prevent and manage high blood pressure. “.
MAYO CLINIC provides information as well about HTN and how to prevent it by:
-“When you eat out, order baked, broiled, steamed or pouched foods without breading or butter or sauces. Also ask that no salt be added. Go easy on the salad dressing. Most are high in salt.
What not to buy:
-Canned Vegetables, sauerkraut. Self rising flour and corn meal. Prepared mixes (waffle, pancake, muffin, cornbread, etc…)
-Dairy Products- like buttermilk (store-bought), canned milks unless diluted and used as regular milk). Egg substitute limit to ½ cup/day. Eggnog (store bought) and salted butter or margarine do not buy.
-Soups: Boullon (all kinds), canned broth, dry soup mixes, canned soups.
-Meats and meat substitutes not to buy= Canned meats, canned fish, cured meats, all types of sausages, sandwich meats, peanut butter, salted nuts.
-Prepared mixes (pie, pudding, cake) or store bought pies, cakes, muffins.
-Cooking ingredients to use low sodium type or limit to 2 tbsp/day=
Catsup, chili sauce, barbeque sauce, mustard, salad dressing.
-Drinks to stay away from Athletic Drinks (such as Gatorade), canned tomato or vegetable juice (unless unsalted).”