“Information from the ongoing COVID-19 pandemic suggests that this virus is spreading more efficiently than influenza, but not as efficiently as measles, which is highly contagious.”
CDC (cdc.org)
“Information from the ongoing COVID-19 pandemic suggests that this virus is spreading more efficiently than influenza, but not as efficiently as measles, which is highly contagious.”
CDC (cdc.org)
Now Let Us Look At 1918-1919 H1N1 Swyne Flu statistics
CDC states: “The 1918 influenza pandemic was the most severe pandemic in recent history. It was caused by an H1N1 virus with genes of avian origin. Although there is not universal consensus regarding where the virus originated, it spread worldwide during 1918-1919. In the United States, it was first identified in military personnel in spring 1918. It is estimated that about 500 million people or one-third of the world’s population became infected with this virus. The number of deaths was estimated to be at least 50 million worldwide with about 675,000 occurring in the United States.”
So H1N1 affected 500 million people 1/3 of the world at that time.
H1N1 by 1918 killed 50 million deaths.
Covid-19 is not even close in numbers. No comparison and there was a lock down 6 weeks in the US for H1N1 1918 to 1919.
The 100-year anniversary of the 1918 pandemic and the 10-year anniversary of the 2009 H1N1 pandemic are milestones that provide an opportunity to reflect on the groundbreaking work that led to the discovery, sequencing and reconstruction of the 1918 pandemic flu virus. This collaborative effort advanced understanding of the deadliest flu pandemic in modern history and has helped the global public health community prepare for contemporary pandemics, such as 2009 H1N1, as well as future pandemic threats. ”
By the numbers of both pandemics this is shown to be true (Covid -19 compared to our deadliest pandemic 1918-1919 Swine Flu=The Spanish Flu doesn’t even come close in numbers of how many affected and killed).
“ Asthma is a condition in which your airways narrow and swell and produce extra mucus. This can make breathing difficult and trigger coughing, wheezing and shortness of breath. For some people, asthma is a minor nuisance where for others it could be a lot worse.”
MAYO CLINIC
Asthma causes a variety of symptoms that can worsen at any time, making breathing difficult. Asthma is a disease that cannot be cured, but it can be managed. Some days you may not have symptoms, but this doesn’t mean your asthma has gone away. Asthma doesn’t have to slow you down. There are things you can do to control your asthma.
Asthma may cause the linings of your airways to get swollen, and the muscles around them can get tight. Sometimes the swelling and tightness get much worse. This is called an exacerbation, or asthma attack. An asthma attack can happen with any kind of asthma. Over time, effects of uncontrolled asthma, such as increased inflammation and asthma attacks, may have long-term effects on your breathing leading to permanent damage to the lining of your airways. Asthma attacks can be serious; that’s why it’s important for you to work with your healthcare provider to control your asthma.
Asthma may be different for different people. Your healthcare provider may identify your type of asthma based on:
Your healthcare provider may assign the type of asthma that you have based on the most severe category listed above.
Intermittent asthma
If your asthma affects you twice a week or less, your asthma may be intermittent. You may need a rescue inhaler up to 2 days per week. It’s the mildest kind of asthma, but it’s not risk free, so be sure to tell your healthcare provider about your symptoms, and find out what you can do to help keep them under control.
Persistent asthma
Unlike intermittent asthma, with persistent asthma you may have symptoms and other limitations more often. Persistent asthma can be mild, moderate, or severe. Sometimes your symptoms may go away on their own. But other times, uncontrolled asthma may get worse. So can the risk of an asthma attack. It’s important to talk to your healthcare provider about your symptoms, and any changes you notice. Your healthcare provider can work with you to help control your asthma symptoms and reduce your risk.
People with mild asthma may have symptoms more than twice a week, but not every day. They may be awakened 3-4 times a month by their asthma or use a rescue inhaler called a SABA more than 2 days a week. They typically have some minor limits to their activities, but have a normal score on breathing tests. People with mild persistent asthma may also have some risk of asthma attacks that require corticosteroids (like prednisone).
If you have mild asthma, your doctor may prescribe a long-term controller medication like low-dose inhaled corticosteroids, as well as your rescue inhaler. When your mild asthma is well controlled, you may not have any symptoms at all, but this doesn’t mean your asthma has gone away.
If you have mild asthma, talk to your healthcare provider to make sure you are getting the right medicines to control your symptoms, and to help avoid asthma attacks. You should ask your healthcare provider what to watch for, and how to prevent an attack.
If you have severe asthma, you’re not alone. With the help of your doctor, severe asthma can be controlled. However, severe asthma affects roughly 5-10% of people with asthma. Uncontrolled severe asthma may include symptoms throughout the day, every day, or waking up every night due to asthma symptoms. You may need a rescue inhaler several times a day. People with severe asthma may have frequent asthma attacks that require oral corticosteroids, sometimes severe enough to send them to a hospital. Severe asthma may cause many limits to daily activities, and low scores on breathing tests.
Some risk factors that can play a part in whether you develop different types of asthma may include pollution, allergies, smoking, obesity, or genetics.
If your asthma is severe and uncontrolled, your healthcare provider may recommend a specialist, like an allergist or a pulmonary specialist (also called a pulmonologist). These doctors are specially trained to treat asthma. They can help you find the right combination of medication and self-care to help manage your
“Preeclampsia is a disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least 5-8% of all pregnancies, it is a rapidly progressive condition characterized by high blood pressure and usually the presence of protein in the urine. Early recognition of preeclampsia symptoms can save your life.”
Preeclampsia Foundation (preclampsiafoundation.org)
“According to the US Centers for Disease Control and Prevention, hemophilia occurs in approximately 1 in 5,000 live births. There are about 20,000 people with hemophilia in the US. All races and ethnic groups are affected. Hemophilia A is four times as common as hemophilia B while more than half of patients with hemophilia A have the severe form of hemophilia. Von Willebrand disease (VWD) is the most common bleeding disorder, affecting up to 1% of the US population.”
National Hemophilia Foundation
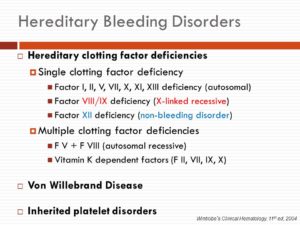
Hereditary clotting factor deficiencies. Single clotting factor deficiency. Factor I, II, V, VII, X, XI, XIII deficiency (autosomal) Factor VIII/IX deficiency (X-linked recessive) Factor XII deficiency (non-bleeding disorder) Multiple clotting factor deficiencies. F V + F VIII (autosomal recessive) Vitamin K dependent factors (F II, VII, IX, X) Von Willebrand Disease. Inherited platelet disorders. Wintrobe’s Clinical Hematology, 11th ed, 2004.
Bleeding disorders are a group of conditions that result when the blood cannot clot properly. In normal clotting, platelets, a type of blood cell, stick together and form a plug at the site of an injured blood vessel. Proteins in the blood called clotting factors then interact to form a fibrin clot, essentially a gel plug, which holds the platelets in place and allows healing to occur at the site of the injury while preventing blood from escaping the blood vessel. While too much clotting can lead to conditions such as heart attacks and strokes, the inability to form clots can be very dangerous as well, as it can result in excessive bleeding. Bleeding can result from either too few or abnormal platelets, abnormal or low amounts of clotting proteins, or abnormal blood vessels.
Hemophilia is perhaps the most well-known inherited bleeding disorder, although it is relatively rare. It affects mostly males.
Many more people are affected by von Willebrand disease, the most common inherited bleeding disorder in America caused by clotting proteins. Von Willebrand disease can affect both males and females. Platelet disorders are the most common cause of bleeding disorder and are usually acquired rather than inherited. You can find information on other bleeding disorders by following the links at the bottom of this page.
How do you know if your at risk?
Bleeding disorders such as hemophilia and von Willebrand disease result when the blood lacks certain clotting factors. These diseases are almost always inherited, although in rare cases they can develop later in life if the body forms antibodies that fight against the blood’s natural clotting factors. Individuals and pregnant women with a family history of bleeding disorders should talk to their doctors about detection and treatment. Symptoms of bleeding disorders may include:
Hemophilia is a rare, inherited bleeding disorder that can range from mild to severe, depending on how much clotting factor is present in the blood. Hemophilia is classified as type A or type B, based on which type of clotting factor is lacking (factor VIII in type A and factor IX in type B). Hemophilia results from a genetic defect found on the X chromosome. Women have two X chromosomes. Women who have one X chromosome with the defective gene are termed carriers and they can pass the disease onto their sons. Due to random chromosome activation, some women carriers may range from asymptomatic to symptomatic depending on how much of their factor VIII or IX is inactivated. In fact, some women may have “mild hemophilia,” though this is less common. Men have one X and one Y chromosome, so if their X chromosome has the defective gene, they will have hemophilia.
Because blood does not clot properly without enough clotting factor, any cut or injury carries the risk of excessive bleeding. In addition, people with hemophilia may suffer from internal bleeding that can damage joints, organs, and tissues over time.
In the past, people with hemophilia were treated with transfusions of factor VIII obtained from donor blood, but by the early 1980s these products were discovered to be transmitting blood-borne viruses, including hepatitis and HIV. Thanks to improved screening techniques, and a major breakthrough that enabled scientists to create synthetic blood factors in the laboratory by cloning the genes responsible for specific clotting factors, today’s factor-replacement therapies are pure and much safer than ever before.
Von Willebrand disease is an inherited condition that results when the blood lacks functioning von Willebrand factor, a protein that helps the blood to clot and also carries another clotting protein, factor VIII. It is usually milder than hemophilia and can affect both males and females. Women are especially affected by von WIllebrand disease during menses. Von Willebrand disease is classified into three different types (Types 1, 2, and 3), based on the levels of von Willebrand factor and factor VIII activity in the blood. Type 1 is the mildest and most common form; Type 3 is the most severe and least common form.
With early diagnosis, people with von Willebrand disease can lead normal, active lives. People with mild cases may not require treatment, but should avoid taking drugs that could aggravate bleeding, such as aspirin and ibuprofen, without first consulting with a doctor. More serious cases may be treated with drugs that increase the level of von Willebrand factor in the blood or with infusions of blood factor concentrates. It is important for people with von Willebrand disease to consult with their doctors before having surgery, having dental work, or giving birth, so that proper precautions can be taken to prevent excessive bleeding. You may be referred to a hematologist, a doctor who specializes in the treatment of blood disorders.
“Hepatitis C and D usually occur as a result of parenteral contact with infected body fluids. Hepatitis A and E are typically caused by ingestion of contaminated food or water.”
Center for Disease Prevention and Control CDC
Hepatitis C is an infectious disease affecting primarily the liver, caused by the hepatitis C virus (HCV). The infection is often asymptomatic, but chronic infection can lead to scarring of the liver and ultimately to cirrhosis, which is generally apparent after many years. In some cases, those with cirrhosis will go on to develop liver failure, liver cancer, or life-threatening esophageal and gastric varices.
HCV is spread primarily by blood-to-blood contact associated with intravenous drug use, poorly sterilized medical equipment, and transfusions. An estimated 150–200 million people worldwide are infected with hepatitis C. The existence of hepatitis C – originally identifiable only as a type of non-A non-B hepatitis – was suggested in the 1970s and proven in 1989. Hepatitis C infects only humans and chimpanzees. It is one of five known hepatitis viruses: A, B, C, D, and E.
The virus persists in the liver in about 85% of those infected. This infection of the liver is caused by the hepatitis virus. About 3.2 million people in the U.S. have the disease. But it causes few symptoms, so most of them don’t know.
There are many forms of the hepatitis C virus. The most common in the U.S. is type 1. None is more serious than any other, but they respond differently to treatment.
Jaundice (a condition that causes yellow eyes and skin, as well as dark urine), Stomach pain, Loss of appetite, Nausea, and Fatigue.
HOW IT’S TRANSMITTED
The virus spreads through the blood or body fluids of an infected person.
You can catch it from:
-Sharing drugs and needles
-Having sex, especially if you have an STD, an HIV infection, several partners, or have rough sex.
-Being stuck by infected needles
-Birth — a mother can pass it to a child
Hepatitis C isn’t spread through food, water, or by casual contact.
HOW IT’S DIAGNOSED
You can get a blood test to see if you have the hepatitis C virus.
Are There Any Long-Term Effects?
Yes. About 75% to 85% of people who have it develop a long-term infection called chronic hepatitis C. It can lead to conditions like liver cancer and cirrhosis, or scarring of the liver. This is one of the top reasons people get liver transplants.
WHAT’S THE TREATMENT:
Hepatitis C treatments have changed a lot in recent years. The latest is a once-daily pill called Harvoni that cures the disease in most people in 8-12 weeks. It combines two drugs: sofosbuvir (Sovaldi) and ledipasvir. In clinical trials, the most common side effects were fatigue and headache. However, the medicine is expensive. Interferon and ribavirin used to be the main treatments for hepatitis C. They can have side effects like fatigue, flu-like symptoms, anemia, skin rash, mild anxiety, depression,nausea, and diarrhea.
THOSE AT HIGHEST RISK:
Certain things may increase your risk of becoming infected with the hepatitis C virus. Just because you are at risk for getting hepatitis C does not mean that you have the virus.
Many people do not know how they became infected with hepatitis C.
Recommended Related to Hepatitis
Tips to Deal With Hepatitis C Fatigue
When you have hepatitis C, being tired — really tired — can be a fact of life. But there are ways you can boost your energy. Here, three people who have experience with fatigue from the disease share their tips.
You can get hepatitis from:
–Sharing needles and other equipment (such as cotton, spoons, and water) used to inject drugs.
-Having your ears or another body part pierced, getting a tattoo, or having acupuncture with needles that have not been sterilized properly. The risk of getting hepatitis C in these ways is very low.
-Working in a health care environment where you are exposed to fresh blood or where you may be pricked with a used needle. Following standard precautions for health care workers makes this risk very low.
HEPATITIS D
Hepatitis D (hepatitis delta) is a disease caused by the hepatitis D virus (HDV), a small circular enveloped RNA virus. This is one of five known hepatitis viruses: A, B, C, D, and E. HDV is considered to be a sub-viral satellite because it can propagate only in the presence of the hepatitis B virus (HBV).
Transmission of HDV: Most already are with Hepatitis B. How can it transmit from one to another? Well similar to that of Hepatitis B including:
Spread through infected Hepatitis B or D needles shared since one of the users blood is infected with the infection.
Spread through a sex partner infected with Hepatitis B or D via the semen
****both spreads infected through the blood and fluids in the body****
Spread through a infected mother to her newborn.
Remember it can occur either via simultaneous infection with HBV (coinfection) or superimposed on chronic hepatitis B or hepatitis B carrier state (superinfection).
Both superinfection and coinfection with HDV results in more severe complications compared to infection with HBV alone. These complications include a greater likelihood of experiencing liver failure in acute infections and a rapid progression to liver cirrhosis, with an increased chance of developing liver cancer in chronic infections. In combination with hepatitis B virus, hepatitis D has the highest fatality rate of all the hepatitis infections, at 20%.
The routes of transmission of hepatitis D are similar to those for hepatitis B. Infection is largely restricted to persons at high risk of hepatitis B infection, particularly injecting drug users and persons receiving clotting, and is mostly associated with intravenous drug use. factor concentrates. Worldwide more than 15 million people are co-infected. HDV is rare in most developed countries
TREATMENT:
The vaccine for hepatitis B protects against hepatitis D virus because of the latter’s dependence on the presence of hepatitis B virus for it to replicate.
Low quality evidence suggests that interferon alpha can be effective in reducing the severity of the infection and the effect of the disease during the time the drug is given, but the benefit generally stops when the drug is discontinued, indicating that it does not cure the disease. Interferon is effective only in ~20% of cases.
The drug myrcludex B, which inhibits virus entry into hepatocytes, is in clinical trials as of October 2015
Hepatitis E virus (HEV) is another liver infection. Hepatitis E is a self-limited disease that does not result in chronic infection. While rare in the United States, Hepatitis E is common in many parts of the world. It is transmitted from ingestion of fecal matter, even in microscopic amounts, and is usually associated with contaminated water supply in countries with poor sanitation is a liver infection caused by the Hepatitis E virus (HEV). Hepatitis E is a self-limited disease that does not result in chronic infection.
Hepatitis E is a common cause of hepatitis outbreaks in developing parts of the world and is increasingly recognized as an important cause of disease in developed countries. Safe and effective vaccines to prevent HEV infection have been developed but are not widely available. There is no FDA approved vaccination for Hepatitis E.
“Hepatitis is an inflammation of the liver. Viruses cause most cases of hepatitis. The type of hepatitis is named for the virus that causes it; for example, hepatitis A, hepatitis B or hepatitis C. Drug or alcohol use can also cause hepatitis. In other cases, your body mistakenly attacks healthy cells in the liver.”
medicineplus.com