Understanding how nerve damage occurs:
Various ideas have been proposed to explain how GBS develops. One explanation is known as the “molecular mimicry/innocent bystander” theory. According to this explanation, molecules on some nerves are very similar to or mimic molecules on some microorganisms. When those microbes infect someone, the immune system correctly attacks them. And if the microbe and myelin look similar, the immune system makes a mistake and attacks the myelin.
Different mechanisms may explain how the molecular mimicry concept may work. When Guillain-Barré syndrome is preceded by a viral or bacterial infection, it is possible that the infecting agent has changed the chemical structure of some nerves. The immune system treats these nerves as foreign bodies and mistakenly attacks them. It is also possible that the virus makes the immune system itself less discriminating and no longer able to recognize its own nerves. Some parts of the immune system—special white blood cells called lymphocytes and macrophages—perceive myelin as a foreign body and attack it. Specialized white blood cells called T lymphocytes (from the thymus gland) cooperate with B lymphocytes (that originate in bone marrow) to produce antibodies against the person’s own myelin and damage it.
In some forms of GBS, antibodies made by the person to fight a Campylobacter jejuni bacterial infection attack axons in the motor nerves. This causes acute motor axonal neuropathy, which is a variant of GBS that includes acute paralysis and a loss of reflexes without sensory loss. Campylobacter infections can be caused by ingesting contaminated food or from other exposures. The infected person’s body then makes antibodies against Campylobacter. Some Campylobacter molecules resemble molecules in the person’s nerve axons, so when the person’s antibodies fight the Campylobacter bacteria they also attack the look-alike axons. This slows nerve conduction and causes paralysis. Scientists are investigating various GBS subtypes to find why the immune system reacts abnormally in this syndrome and other autoimmune diseases.
Guillian Barre Syndrome (GBS) is associated with cranial nerve involvement. Commonest cranial nerves involved were the facial and bulbar (IXth and Xth) .Guillian Barre Syndrome (GBS) is associated with cranial nerve involvement. Most common cranial nerves involved are the facial and bulbar (IXth and Xth). Involvement of twelfth cranial nerve is rare in GBS. Your hypoglossal nerve is the 12th cranial nerve which is responsible for the movement of most of the muscles in your tongue. It starts in the medulla oblongata and moves down into the jaw, where it reaches the tongue. .
What disorders are related to GBS?
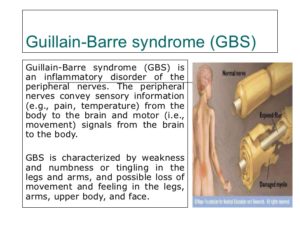
Guillain-Barré syndrome is one of several disorders involving weakness due to peripheral nerve damage caused by the person’s immune system. While GBS comes on rapidly over days to weeks, and the person usually recovers, other disorders develop slowly and can linger or recur.
The most common type of GBS seen in the United States is acute inflammatory demyelinating polyneuropathy (AIDP). In AIDP, the immune response damages the myelin coating and interferes with the transmission of nerve signals. In two other types of Guillain-Barré syndrome, acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN), the axons themselves are damaged by the immune response.
Miller-Fisher syndrome is a rare, acquired nerve disease that is a variant of Guillain-Barré syndrome. It is characterized by abnormal muscle coordination with poor balance and clumsy walking, weakness or paralysis of the eye muscles, and absence of the tendon reflexes. Like GBS, symptoms may follow a viral illness. Additional symptoms include generalized muscle weakness and respiratory failure. Most individuals with Miller Fisher syndrome have a unique antibody that characterizes the disorder.
Related peripheral nerve disorders with slow onset and persisting or recurrent symptoms include chronic inflammatory demyelinating polyneuropathy (CIDP) and multifocal motor neuropathy. CIDP features weakness that can recur, repeatedly, over the course of years. Multifocal motor neuropathy typically affects many different muscles in a small part of a limb or limbs. Usually the symptoms are more severe on one side of the body.
Stay tune for Part III on GBS regarding how its diagnosed and the Rx including rehab.