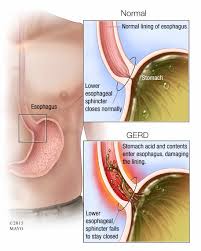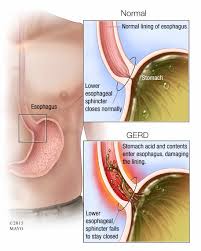

How to stay healthy with acid reflux? A GI disease that is caused by a valve located between the esophagus and stomach, which normally is a strong muscular ring of tissue. This valve normally opens and closes completely preventing food backing up (called reflux) in the esophagus allowing the contents to reach the throat to the mouth. With acid reflux, what happens is this valve gets over expanded frequently to the point the valve gets overstretched and no longer fits over the opening between the esophagus and the stomach with a tight fit. Due to loss of the elasticity it now is allowing leakage from the stomach with both food and fluids going up the esophagus to the throat to the mouth due to the action of reflux, during the digestion process. What happens during digestion the stomach contents with digestive fluids (which are acidic) are refluxed, that are not normally in the esophagus. In conclusion, reflux sends stomach contents that’s returning (an acidic environment) upward in the esophagus which is now in an environment not use to being exposed to the digestive fluids =acidity, which are needed to perform the digestion process of our foods/fluids that are in the stomach only. This leakage of the valve is the cause of this problem occurring=GERD or gastrointestinal reflux.
When you don’t have GERD food and fluids when swallowed go down the esophagus to the valve where it opens letting the contents into the stomach, where digestion takes place in about 1-2 hours after eating. Normally the valve is tight enough in preventing reflux=no leakage (the primary purpose of its function). This means during digestion the food gets into the stomach which is broken down into smaller particles by the digestive acid fluids allowing the nutrients to pass into the bloodstream with the waste products staying in the stomach but when stomach digestion is complete it passes all the waste products onto the smaller intestines to the larger intestines to the rectum to be evacuated, without leakage or reflux.
The signs and symptoms (s/s) of GERD or acid reflux:
1-Heartburn is the classic GERD symptom. It’s best described as a burning sensation in the chest and/or discomfort in the upper belly or abdomen accompanied by a feeling of fullness.
2- Regurgitation is the involuntary return of partially digested food from the stomach into the mouth. This uncomfortable symptom is commonly caused by GERD, since the esophageal sphincter (valve) is damaged to such a severe degree that the stomach juices (acidotic) can freely reflux to the level of the throat or mouth.
3-Pain present behind the sternum (chest pain) to the upper mid abdomen (where the stomach is). If severe call your M.D. or doctor to have evaluated (especially if in the chest).
4-Chronic cough to hoarseness 5-Recurrent pneumonias 6-Bloating 7-Nausea 8-Vomiting (yellow/green) 9-Lump in the throat 10-Difficulty swallowing 11-Chronic sore throat 12-Laryngitis 13-Post nasal drip 14-Ear Aches 15-Tooth decay or gingivitis (inflammation of the gums) or bad breath this is due to the acid fluids with the foods and fluids regurgitated back to the mouth from the stomach.
Complications that are caused by GERD when left untreated:
1-Narrowing of the esophagus called esophageal stricture. This is due to damage to cells in the lower esophageal from acid exposure that leads to scarring of the tissue. The scar tissue narrows the food pathway causing difficulty to swallow called dysphagia. 2-Esophagitis – inflammation of the esophagus. This constant backwash of acid can irritate the lining of your esophagus. Over time, the inflammation can cause complications such as bleeding or breathing problems leading into esophagitis.
3-Esophageal Ulcers – Due to frequent exposure to acidic fluids and foods to the esophagus the mucosa gets irritated so bad it will even erode the mucosa causing skin ulceration. The esophagus environment is not use to the stomach’s = acidic. Take the outer skin of the body, if exposed long enough to acidic chemicals the skin will burn. Same principle for the esophagus constantly exposed to the environment of the stomach’s content of acidic fluids every time digestion takes place.
4-Precancerous changes to the esophagus (Barrett’s esophagus). In Barrett’s esophagus, the color and composition of the tissue lining the lower esophagus change. These changes are associated with risk of esophageal cancer. The risk of cancer is low. Cancer is rare but can happen (adenocarcinoma of the esophagus).
Risk factors=Conditions that increase the risk of GERD would include: Obesity, Pregnancy, Smoking, Dry Mouth, Diabetes, Asthma, Connective Tissue Disorders like scleroderma, delayed stomach empting, Zollinger-Ellison syndrome (ZES)
(This is a rare disorder characterized by one or more tumors in the pancreas, duodenum, or both. The tumors cause the stomach to make too much acid, leading to peptic ulcers in the duodenum. The tumors are sometimes cancerous and spread to other areas of the body.).
The key to treatment is prevention but if already with the Dx: GERD than it would be maintenance. There is no one answer but start with being checked by your physician if you have any symptoms indicative of this diagnosis. Start with a getting a very good diagnostic tool ordered by your doctor called an Upper GI series (endoscopy) and when it’s done it will tell the M.D. a lot in what’s going on. Then there is medications as a remedy, that can be useful, they are classified as proton pump inhibitors to H2 Inhibitors with more. Another great key to the treatment is your LIFESTYLE=Diet (not eating acid foods, not eating fast), activity/exercise, your height compared to your weight (BMI or simply what you weigh) and lastly if you practice healthy vs. unhealthy habits. If you would like to learn more about this come back tomorrow to my web page when I go further on the topic GERD (part 2) regarding the diet for the disease.