What is cleft lip and palate?
National Cleft and Craniofacial Awareness and Prevention Month is observed in July. This is an opportunity to raise awareness and improve understanding of orofacial clefts, clefts of the lip and palate, and other conditions of the head and face. In the United States, approximately 2,600 babies are born with a cleft palate and 4,400 babies are born with a cleft lip, with or without a cleft palate each year. There are other craniofacial birth defects including craniosynostosis (skull sutures fusing prematurely), anotia/microtia (ear is missing or underdeveloped), and anophthalmia/microphthalmia (missing or abnormally small eye).
There are several forms of cleft lip and palate, and each one requires a slightly different treatment. The three types of cleft lip and palate are
- Unilateral incomplete
- Unilateral complete
- Bilateral complete
What causes cleft lip and cleft palate?
We’re not sure what causes cleft lip and cleft palate. They may be caused by a combination of factors, like genes and things in your everyday life, like certain medicines you take. Risk factors include:
- Having a family history of cleft lip and cleft palate
- Smoking or drinking alcohol during pregnancy
- Having diabetes before pregnancy
- Taking certain anti-seizure medicines during the first trimester of pregnancy, like topiramate or valproic acid
- Being obese during pregnancy.
- Having certain infections during pregnancy, like rubella (also called German measles)
How are Cleft lip and palate treated?
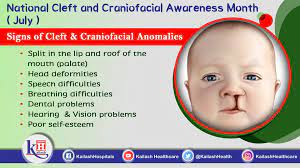
Cleft lip and palate can cause problems with speech, eating, hearing, and social development. Most of the time, cleft lip and palate can be easily treated with corrective surgery, allowing children born with the condition to live normal lives. However, in some cases – particularly in developing countries where access to medical care is not as widely available – children do not receive treatment. This can result in further problems as the child grows.
July is National Cleft and Craniofacial Awareness and Prevention Month.
Cleft lip and cleft palate happen when a baby’s lip or mouth doesn’t form completely during pregnancy. Cleft lip is an opening in a baby’s upper lip. Cleft palate is an opening in the roof of a baby’s mouth. Cleft lip and cleft palate are birth defects. These conditions affect thousands of babies, children, teens and adults in the United States each year.
Cleft lip and palate happen very early in pregnancy. Your baby’s lips form between 4 and 7 weeks of pregnancy, and the palate forms between 6 and 9 weeks of pregnancy. Cleft lip and palate don’t have to happen together — a baby can have one without the other.
Prevention:
To help reduce the chances of having a baby with an orofacial cleft or other craniofacial condition health care providers must encourage patients who are thinking about becoming pregnant to commit to a healthy lifestyle. Among certain healthy habits, we have: control diabetes, quit smoking, exercise regularly, practice yoga, etc. before becoming pregnant. Moreover, health care providers should also work with prospective parents to make informed decisions about medical treatment during pregnancy. This condition can occur in the first three months of pregnancy. Therefore, steps before becoming pregnant are essential for the health of the baby.