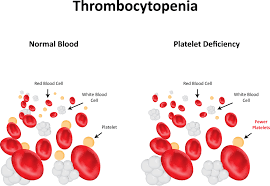
Thrombocytopenia is a condition in which you have a low blood platelet count. Platelets (thrombocytes) are colorless blood cells that help blood clot. Platelets stop bleeding by clumping and forming plugs in blood vessel injuries.
Thrombocytopenia often occurs as a result of a separate disorder, such as leukemia or an immune system problem. Or it can be a side effect of taking certain medications. It affects both children and adults.
Thrombocytopenia may be mild and cause few signs or symptoms. In rare cases, the number of platelets may be so low that dangerous internal bleeding occurs. Treatment options are available.
SIGNS AND SYMPTOMS OF THROMBOCYTOPENIA:
- Easy or excessive bruising (purpura)
- Superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots (petechiae), usually on the lower legs
- Prolonged bleeding from cuts
- Bleeding from your gums or nose
- Blood in urine or stools
- Unusually heavy menstrual flows
- Fatigue
- Enlarged spleen
- Jaundice
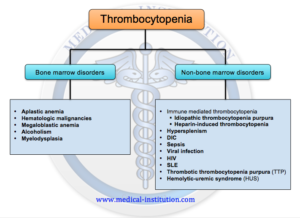
What causes Thrombocytopenia:
If for any reason your blood platelet count falls below normal, the condition is called thrombocytopenia. Normally, you have anywhere from 150,000 to 450,000 platelets per microliter of circulating blood. Because each platelet lives only about 10 days, your body continually renews your platelet supply by producing new platelets in your bone marrow.
Thrombocytopenia can be inherited or it may be caused by a number of medications or conditions. Whatever the cause, circulating platelets are reduced by one or more of the following processes: trapping of platelets in the spleen, decreased platelet production or increased destruction of platelets.
This could be conditions causing your thrombocytopenia:
INFECTIONS:
- Viral infections, including chickenpox, parvovirus, hepatitis C, Epstein-Barr, and HIV, systemic lupus erythematosus (SLE), chronic lymphocytic leukemia (CLL) and drug-induced immune thrombocytopenia
- Sepsis, a severe bacterial infection in your blood
- Helicobacter pylori (H. pylori), a bacteria that can live in your digestive system
MEDICINES:
- Medication side effects, including drugs for heart problems, seizures, and infections
- Heparin, a blood thinner used to prevent blood clots
- Chemotherapy
OTHER TREATMENTS: Heart bypass surgery and Radiation treatment on your bone marrow.
MEDICAL CONDITIONS:
- Blood cancer such as leukemia or lymphoma
- A problem with your bone marrow, like toxicity from excessive alcohol use
- Vitamin B12 or folate (vitamin B9) deficiency
- Pregnancy. Up to 5% of healthy women get it during pregnancy, and it usually gets better on its own after your baby is born. But it can also be a sign of something more concerning, like preeclampsia or HELLP syndrome.
- An enlarged spleen
- Your body uses too many platelets, leaving you without enough of them. That can happen if you have an autoimmune disease, like rheumatoid arthritis or lupus.
- Rare disorders like hemolytic uremic syndrome and thrombotic thrombocytopenic purpura (TTP), which uses a lot of platelets to make small blood clots throughout your body.
TESTS TO HELP DIAGNOSE THROMBOCYTOPENIA:
Physical exam, including a complete medical history. Your doctor will look for signs of bleeding under your skin and feel your abdomen to see if your spleen is enlarged. He or she will also ask you about illnesses you’ve had and the types of medications and supplements you’ve recently taken.
CBC ( complete blood count ). This measures the number of your red and white blood cells and platelets.
Blood smear. This shows how your platelets look under a microscope.
Bone marrow test . Your doctor uses a very fine needle to draw a small amount of liquid bone marrow and check it for cells that may not be working right. Or you may get a biopsy using a different kind of needle, so your doctor can check the types and numbers of cells in the bone marrow.
You may need more tests to help your doctor figure out what’s going on.