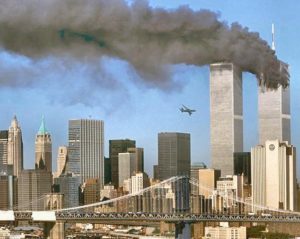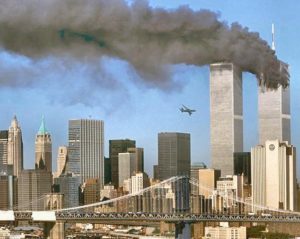




HEALTH EFFECTS FROM SEPTEMBER 11 DISASTER
The world trade center (WTC) terrorist attact and its aftermath exposed hundreds of thousands of people to dust, debris, smoke and fumes. I was one that went down that day as a volunteer RN to help out my country. It was a sight I will never forget and thank God nothing like it has happened since including developing anything from being exposed to the environment of this disaster. September 11, 2001, among rescue and clean up workers, office workers, building evacuees, and residents of lower Manhattan living down their have shown increased respiratory and other physical health problems, like developing cancers after this terrible terrorist tragedy. Following is a outline of the most common conditions experienced by individuals exposed to the WTC attacks and their aftermath. The types of conditions are:
Upper Airway Cough Syndrome: Formerly named postnasal drip syndrome which is commonly caused by continuous irritation or infection of the sinuses and the nose either due to allergies or from environmental irritants. The signs or symptoms that arise from this are cough, nasal congestion, postnasal drip and frequent need to clear the throat.
Asthma/Reactive Airways Dysfunction Syndrome: Some people exposed to the WTC disaster area have developed asthma related to exposure to irritants (also called reactive airways dysfunction syndrome [RADS]). Signs and symptoms include: Shortness of Breath (SOB); chest tightness, wheezing, coughing, phlegm, possible triggering of symptoms by colds or seasonal allergies or exercise or fragrances or extremes of temperature or humidity, recurrent episodes of respiratory infections requiring antibiotic treatment.
GASTROESOPHAGEAL REFLUX DISEASE OR LARYNGOPHARYNGEAL REFLUX DISEASE: Some people exposed to the WTC disaster developed this condition. GERD results from the flow back or return (reflux) of stomach contents into the esophagus. LPRD results from the reflux of stomach contents into the voice box or throat.
Symptoms of GERD: Heartburn, acid regurgitation, upset stomach, cough made worse with meals or at night
Symptoms of LPRD: Hoarseness or other vocal changes, sore throat, cough, sensation of having a lump in the throat
Long-Term Physical Health Concerns
There has been increased concern about sarcoidosis and cancer among individuals who were highly exposed during the WTC disaster. The NYC Department of Health and Mental Hygiene, in conjunction with other programs, is closely monitoring these conditions in order to detect any increases in these diseases.
At this time, there is no evidence of an increased rate of cancer among individuals highly exposed to the WTC disaster. Increased rates of sarcoidosis have been documented among fire department personnel ( Izbicki G, Chavko R, Banauch, GI, et al. World Trade Center “Sarcoid-Like” Granulomatous Pulmonary Disease in New York City Fire Department Workers. Chest. 2007;3:131;1414-1423). Rates of sarcoidosis among other groups are currently under investigation.
Sarcoidosis is difficult to verify because NYC providers are not required by law to report sarcoidosis cases to the Health Department. Based on New York City death certificate records over the past 10 years, there have been an average of 32 sarcoidosis deaths per year, with the annual number remaining the same since the WTC attacks. During the same period, there have been between 362 and 439 sarcoidosis-related hospitalizations per year in NYC (five per 100,000 people), with the annual rate remaining the same since the disaster.
* Breathing in beryllium, other metal dust or fumes or moldy materials can cause lung disease, which may resemble sarcoidosis.
.Sarcoidosis
Sarcoidosis* is an auto-immune disease that can attack any organ of the body, although it often starts in the lungs or lymph nodes. It mainly affects people between 20 and 40 years of age, with African-Americans three times more likely to develop the condition than Caucasians and women twice as likely to develop it as men. While most sarcoidosis patients recover without treatment, less than one-third develop chronic debilitating sarcoidosis and fewer than 5% die from the disease. The exact cause of sarcoidosis is unknown.
Sarcoidosis and World Trade Center (WTC) Dust Exposure
While studies have not definitively linked dust exposure from the WTC disaster to new-onset sarcoidosis among exposed workers, the data does suggest elevated levels of sarcoidosis among firefighters.
There have been a few reported sarcoidosis cases among rescue workers that may be related to Ground Zero dust exposure. In May 2007, the New York City Chief Medical Examiner determined that dust exposure from the disaster contributed to a sarcoidosis death, based on published epidemiologic findings among exposed firefighters.
Cancers
The collapse and burning of the WTC and neighboring buildings released a complex mixture of irritant dust, smoke and gases. The dust cloud also contained heavy metals, as well as asbestos and other carcinogens. In addition, smoke released from the fires contained hazardous and potentially cancer-causing substances.
Because of these exposures, there has been concern about the possibility of increased cancer rates among WTC-exposed people. The NYC Department of Health and Mental Hygiene, the Fire Department of New York and other researchers are carefully monitoring cancer rates among highly exposed people.
In 2007, the NYC Department of Health and Mental Hygiene brought together a panel of experts, including representatives from FDNY, the Mount Sinai School of Medicine, the New York State Department of Health and the National Institute for Occupational Safety and Health, to discuss the potential impact of the WTC disaster on cancer rates and mortality.
In 2010, after beginning the process of confirming cancer diagnoses within their cohorts, the NYC Department of Health and Mental Hygiene and FDNY co-chaired another conference of outside experts, including biostatisticians, environmental health scientists and cancer epidemiologists, to help address the complex methodological questions associated with their preliminary cancer investigations. The conference produced several recommendations which are described in the 2010 WTC Medical Working group annual report.
Although cancer associated with specific exposures takes a long time to develop, three early cancer studies based on verified diagnoses within their cohorts through 2008 (the latest year for which data was available when these analyses began) have been published:
- FDNY found that nearly 9,000 firefighters with WTC exposure may be at greater risk for cancer than firefighters who weren’t exposed.
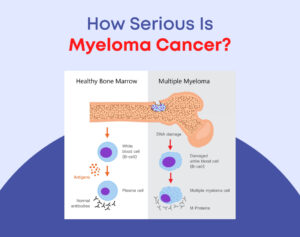
- The WTC Health Registry found small increases in rates of prostate cancer, thyroid cancer and multiple myeloma, a blood cancer, among nearly 34,000 WTC rescue and recovery workers in comparison to rates among New York State residents after adjusting for age, race/ethnicity and sex.
- Prostate and thyroid cancer rates were higher than expected among nearly 21,000 rescue and recovery workers enrolled in the WTC Health Program in comparison to rates in New York, New Jersey, Connecticut and Pennsylvania where the majority of workers lived.
Cancer analyses continue at FDNY, the WTC Health Registry and at the Mount Sinai School of Medicine.
In 2012, the National Institute for Occupational Safety and Health added many different types of cancers to the list of conditions that can be treated at the World Trade Center Health Program.
What the New York City Health Department Is Doing:
Through the World Trade Center (WTC) Health Registry, the Health Department is conducting a cancer study that will help determine if cancer rates are higher among those exposed to the WTC disaster. Results of the study will appear on this Web site and will be submitted to peer-reviewed scientific journals.
The Department is also conducting a broader public awareness campaign about cancer testing, and is working with its clinical partners to offer free cancer screenings. Identifying cancer early in the course of the disease reduces the risk of developing disability from cancer. Department efforts to reduce the rates of smoking among WTC disaster-exposed people also help reduce their risk for developing cancer and other diseases.
What You Can Do
Seek medical care.
If you were exposed to the WTC disaster and have developed symptoms or conditions you feel are related to this exposure, tell your doctor and bring the Clinical Guidelines for Physicians Treating Adults Exposed to the WTC Disaster to help your doctor diagnose and treat your symptoms. The Health Department also released clinical guidelines for health care providers on how to treat children and adolescents exposed to the WTC disaster.
If you or your doctor believe that you require more specialized care, you may be eligible for free treatment at a WTC Center of Excellence or affiliated facility.
Practice preventive health.
Whether or not you are currently experiencing symptoms, there are things you can do to maintain your current health status, prevent worsening of your health, and detect any new conditions. Suggested measures include:
-
- If you smoke, quit! Tobacco is known to cause cancer and make existing respiratory conditions worse. If you currently smoke, there are programs in place to help you quit.
- Lead a healthy lifestyle by drinking alcohol in moderation and avoiding more than moderate sun exposure. Increase physical activity, keep your weight down and eat a healthful and nutritious diet.
- Have a physical exam every year that includes a complete blood count (CBC). Be sure your exam includes all tests appropriate for your sex and age, including cancer screenings.
- Avoid risks at work and during leisure time. If you have any respiratory conditions try to reduce your exposure to irritants such as dust, pollen, grass and smoke both at home and at work. Consider giving up activities that expose you to irritants, and if activities cannot be avoided, wear personal protective equipment to minimize exposure.