Today’s topics will be covering on leukemia and lymphoma than what is the difference between them actually. It will also include the factors proning you to these cancers, the tests that the M.D. might do and the different treatments for all 3 cancers Leukemia, Lymphoma and Myeloma (discussed in Part II).
Leukemia
Leukemia and Lymphoma Society states leukemia begins in a cell in the bone marrow and in the blood. Remember the bone marrow creates our cells releasing them into the blood stream. The cell undergoes a change and becomes a type of leukemia cell. Once the marrow cell undergoes a leukemic change, the leukemia cells may grow and survive better than normal cells. Over time, the leukemia cells crowd out or suppress the development of normal cells. The rate at which leukemia progresses and how the cells replace the normal blood and marrow cells are different with each type of leukemia.
After diagnosis and treatment, many people with leukemia live many good, quality years.
Leukemia is a cancer of the early blood-forming cells, meaning just coming formed from the bone marrow. Most often, leukemia is a cancer of the white blood cells, but some leukemia (s) start in other blood cell types or effect the count of other cells in our bloodstream. Leukemia is often described as being either acute (fast growing) or chronic (slow growing). Different types of leukemia have different treatment options and outlooks.
The National Cancer Institute also says leukemia is a broad term for cancers of the blood cells. The type of leukemia depends on the type of blood cell that becomes cancer and whether it grows quickly or slowly. Leukemia occurs most often in adults older than 55, but it is also the most common cancer in children younger than 15.
Leukemia may affect red blood cells, white blood cells, and platelets.
In a healthy child, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell.
A myeloid stem cell becomes one of three types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- Platelets that form blood clots to stop bleeding.
- White blood cells that fight infection and disease.
A lymphoid stem cell becomes a lymphoblast cell and then one of three types of lymphocytes (white blood cells):
- B lymphocytes that make antibodies to help fight infection.
- T lymphocytes that help B lymphocytes make the antibodies that help fight infection.
- Natural killer cells that attack cancer cells and viruse
The major types of leukemia are:
- Acute lymphocytic leukemia (ALL). This is the most common type of leukemia in young children. ALL can also occur in adults.
- Acute myelogenous leukemia (AML). AML is a common type of leukemia. It occurs in children and adults. AML is the most common type of acute leukemia in adults.
- Chronic lymphocytic leukemia (CLL). With CLL, the most common chronic adult leukemia, you may feel well for years without needing treatment.
- Chronic myelogenous leukemia (CML). This type of leukemia mainly affects adults. A person with CML may have few or no symptoms for months or years before entering a phase in which the leukemia cells grow more quickly.
- Other types. Other, rarer types of leukemia exist, including hairy cell leukemia, myelodysplastic syndromes and myeloproliferative disorders.
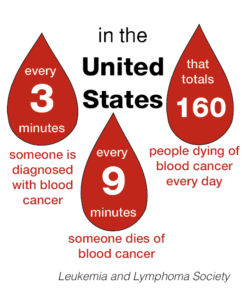
Statistics by the American Cancer Society: Leukemia is the most common type of cancer in children and teens, accounting for 1 out of 3 cancers. Most childhood leukemias are ALL Acute Lymphocytic Leukemia. Most of the remaining cases for childhood are AML Acute Myeloid Leukemia. Chronic Leukemia is rare in children. However, because other types of leukemia become more common with age, most leukemia is found in among adults.
Decades of research have led to vastly improved outcomes for children diagnosed with ALL.
Lymphoma
Lymphoma starts in the immune system and affects the lymph nodes and lymphocytes, which are a type of white blood cell. There are two main types of lymphocyte, B cells and T cells. Whereas Leukemia starts in the bone marrow affecting the white blood cells. Doctors categorize leukemia based on which type of white blood— lymphocytes or myeloid cells — and whether the illness is developing very quickly (acute disease) or slowly over time (chronic disease).
Cancer can affect any part of the body, including the blood. Leukemia and lymphoma are both forms of blood cancer. The main difference is that leukemia affects the blood and bone marrow, while lymphomas tend to affect the lymph nodes. BUT remember leukemia can go into the lymph nodes since its in the blood stream the cancer cells and can effect the lymph nodes. BOTH effect white blood cells. Myeloma is similar in that it effects plasma a white blood cell.
The origin of where Myeloma, Leukemia or Lymphoma. Lets look at all 3 All start in the Bone Marrow but the effect is similar in general but the type with the stage of cancer the individual has is a major factor of ending results.
All 3 types of cancers this article in Part I to Part II are bad cancer cells that derive in all in the bone marrow and they all effect some type of White Blood Cell (WBC). All White Blood Cells are to fight infection and prevent it.
Myeloma effects the normal plasma cells originating in the bone marrow and are an important part of the immune system. Lymphocytes (lymph cells) are one of the main types of white blood cells in the immune system and include T cells and B cells. Lymphocytes are in many areas of the body, such as lymph nodes, the bone marrow, the intestines, and the bloodstream. These are the cells involved in this cancer being the problem.
Lymphoma is cancer that begins in infection-fighting cells of the immune system, called lymphocytes. Leukocytes are WBCs also that are affected in this cancer like Myeloma. In Lymphoma the leukocytes become an abnormal amount (of WBCs) in the body. Lymphocytes are a form of small leukocyte (white blood cell) with a single round nucleus (remember this is the brain for the cell), occurring especially in the lymphatic system. Abnormal lymphocytes, a type of white blood cell that fights infection, become lymphoma cells, which multiply and collect in your lymph nodes. Over time, these cancerous cells impair your immune system. Lymphomas are divided into two categories: Hodgkin lymphoma and non-Hodgkin lymphoma (this is another topic in itself). These cells are in the lymph nodes, spleen, thymus, bone marrow, and other parts of the body.
Leukemia is a cancer of the body’s blood-forming tissues, including the bone marrow and the lymphatic system. In Leukemia many of the white blood cells produced in the bone marrow do not mature normally. These abnormal cells, called leukemic cells, are unable to fight infection the way healthy white cells can. As they grow in number, the leukemic cells also interfere with the production of other blood cells. Obviously the WBCs start in the bone marrow just like every cell does.
So these 3 cancers are similar in many ways with the ending results but where they effect initially or their primary area effected might be slightly different, as discussed already in this topic.
Factors that may increase your risk of developing some types of any 3 cancers include:
- Previous cancer treatment. People who’ve had certain types of chemotherapy and radiation therapy for other cancers have an increased risk of developing certain types of leukemia.
- Genetic disorders. Genetic abnormalities seem to play a role in the development of leukemia. Certain genetic disorders, such as Down syndrome, are associated with an increased risk of leukemia.
- Exposure to certain chemicals. Exposure to certain chemicals, such as benzene — which is found in gasoline and is used by the chemical industry — is linked to an increased risk of some kinds of leukemia.
- Smoking. Smoking cigarettes increases the risk of acute myelogenous leukemia.
- Family history of leukemia. If members of your family have been diagnosed with leukemia, your risk of the disease may be increased.
However, most people with known risk factors don’t get leukemia. And many people with leukemia have none of these risk factors.
Regarding Myeloma, Leukemia or Lymphoma:
Doctors may find in a routine blood test, before symptoms begin. If this happens, or if you have signs or symptoms that suggest any 3 of the cancers, you may undergo the following diagnostic exams:
- Physical exam. Your doctor will look for physical signs of Myeloma or Leukemia or Lymphoma, such as pale skin from anemia, swelling of your lymph nodes, and enlargement of your liver and spleen.
- Blood tests. By looking at a sample of your blood, your doctor can determine if you have abnormal levels of red or white blood cells or platelets — which may suggest leukemia.
- Bone marrow test. Your doctor may recommend a procedure to remove a sample of bone marrow from your hipbone. The bone marrow is removed using a long, thin needle. The sample is sent to a laboratory to look for leukemia cells. Specialized tests of your cancer cells that may reveal certain characteristics that are used to determine your treatment options.
Treatment
Treatment for your Myeloma, Leukemia or Lymphoma depends on many factors. Your doctor determines your treatment options based on your age and overall health, the type of cancer of the 3 you have, and whether it has spread to other parts of your body, including the central nervous system.
Common treatments used to fight these 3 blood cancers include:
- Chemotherapy. Chemotherapy is the major form of treatment for all 3. This drug treatment uses chemicals to kill cancer cells.Depending on the type of cancer you have, you may receive a single drug or a combination of drugs. These drugs may come in a pill form, or they may be injected directly into a vein.
- Biological therapy. Biological therapy works by using treatments that help your immune system recognize and attack cancer cells.
- Targeted therapy. Targeted therapy uses drugs that attack specific vulnerabilities within your cancer cells.For example, the drug imatinib (Gleevec) stops the action of a protein within the leukemia cells of people with chronic myelogenous leukemia. This can help control the disease.
- Radiation therapy. Radiation therapy uses X-rays or other high-energy beams to damage cancer cells and stop their growth. During radiation therapy, you lie on a table while a large machine moves around you, directing the radiation to precise points on your body.You may receive radiation in one specific area of your body where there is a collection of cancer cells, or you may receive radiation over your whole body. Radiation therapy may be used to prepare for a stem cell transplant.
- Stem cell transplant. A stem cell transplant is a procedure to replace your diseased bone marrow with healthy bone marrow.Before a stem cell transplant, you receive high doses of chemotherapy or radiation therapy to destroy your diseased bone marrow. Then you receive an infusion of blood-forming stem cells that help to rebuild your bone marrow.You may receive stem cells from a donor, or in some cases you may be able to use your own stem cells. A stem cell transplant is very similar to a bone marrow transplant.