Risk factors for alcohol use disorder include:
- Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can lead to alcohol-related problems or alcohol use disorder.
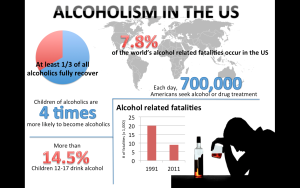
- People who begin drinking at an early age, and especially in a binge fashion, are at a higher risk of alcohol use disorder. Alcohol use may begin in the teens, but alcohol use disorder occurs more frequently in the 20s and 30s. However, it can begin at any age.
- Family history. The risk of alcohol use disorder is higher for people who have a parent or other close relative who has problems with alcohol. This may be influenced by genetic factors.
- Depression and other mental health problems. It’s common for people with a mental health disorder such as anxiety, depression, schizophrenia or bipolar disorder to have problems with alcohol or other substances.
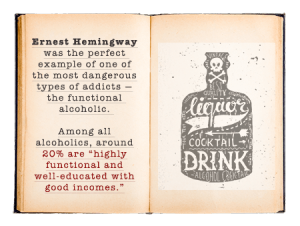
- Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcohol use disorder. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it’s OK to drink too much. For young people, the influence of parents, peers and other role models can impact risk.
Alcohol intoxication results as the amount of alcohol in your blood stream increases. The higher the blood alcohol concentration is, the more impaired you become. Alcohol intoxication causes behavior problems and mental changes. These may include inappropriate behavior, unstable moods, impaired judgment, slurred speech, impaired attention or memory, and poor coordination. You can also have periods called “blackouts,” where you don’t remember events. Very high blood alcohol levels can lead to coma or even death.
Alcohol withdrawal can occur when alcohol use has been heavy and prolonged and is then stopped or greatly reduced. It can occur within several hours to four or five days later. Symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping, nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures. Symptoms can be severe enough to impair your ability to function at work or in social situations.
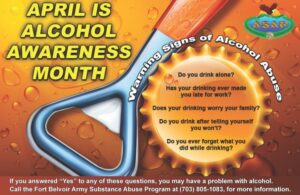
Are you wondering if you drinking is on the high side or it crossed a line into a problem? It may be time to make some changes and its never too LATE!
What could be telling you that your having a problem with drinking? Well if you are asking yourself any of the listed problems or asking yourself the followng questions listed below it maybe time to be checked or you get help:
1. You drink more than planned. If your coming into this situation drinking more than you planned to or longer than you thought than you are having problem controlling your alcohol!
2. You find yourself spending a long time drinking, even getting sick from the drinking but and in time from the side effects of drinking recover. Why even get to that point. Keep track of your daily activities with seeing how often you drink in a diary and see if the bottles add up highier than one glass of wine a day or one or three glasses a week of alcohol. Again you might see it adds up much higher than that.
3. Has your tolerance build up that you have to drink more for your buzz. Your brain adapts over time to alcohol sensitivity and goes up when drinking high levels of alcohol. Just like a completely different disease but similar concept. In a pt without emphysema (COPD type the worst) where in time the brain adjusts to CO2 – Carbon Dioxide levels with O2 levels. A person without emphysema the brain makes us breath on low 02 levels but with a emphysema pt the brain makes them breath based on low CO2 levels since in time the brain developed sensitivity to it.
4. You crave alcohol frequently, another factor in making you want to seek help. There are times you want to drink so badly bases on emotions or physical feelings you are experiencing that can trigger the craving. You can be at a place (like a bar) triggering that craving. That strong need or urge to drink can be triggered by people, places, things also. When you have a trigger reacts to these factors differently than a social drinker’s does.
5. You give up activities; what do you do for fun besides drinking? Now yes life does change but what have you edged out of your life for drinking and or does everything you do entail a lot of drinking. Has drinking stopped you from doing those things you use to do or pushed them out of your life.
6. Are dropping the ball on life? Take work, how many times have you come to work with a hang over, missed dead lines for your boss, or got behind on college work? Now if your drinking in high school you know your under the age and its against the LAW! When your drinking keeps you home sick or from your responsibilities that is a problem!
7. Is it causing friction in your relationships? If you care about your loved ones but can’t imagine your life without drinking that is a problem! If your in this situation, this does not make you a bad person at all but like any problem you need to resolve it. You need to look for help and make changes to help the relationship you have with a significant one in your life or with family members or friends to get those relationships back on the right track for both of you.
8. Are you having Withdrawal S/S from drinking? (S/S are listed above under withdrawal). Remember alcohol changes your brain’s chemistry. When you drink heavy over a long period of time the brain has adapted to the high alcohol in your body. So understand, if you suddenly stop drinking your brain has to adjust again and with doing so this will make withdrawal s/s occur.
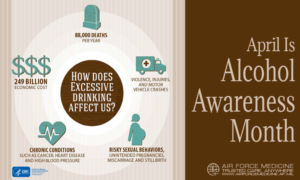
9. Have you been put in the situation that you could have been hurt due to drinking or has an injury actual already happened. Your brain didn’t react fast enough or was it from poor decision making that an injury almost occurred or actually happened (Examples of getting into risky situations due to your heavy drinking could be: Driving, swimming, getting into fights, poor sex-ending up with sexual transmitted diseases or passing on your STD like HIV for example and walking into dangerous areas getting hurt or someone else hurt.)
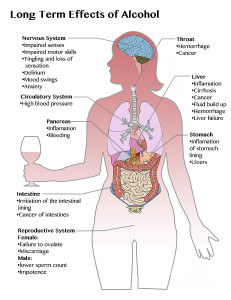
10. Getting sick with medical conditions or health problems due to your heavy drinking. Alcohol can damage your liver, brain, heart, pancreas and even immune system. It can even raise odds of getting certain cancers.
Drinking alcohol increases the risk of cancer. Drinking alcohol doesn’t mean that you’ll definitely get cancer, but the risk is higher the more alcohol you drink.
People might talk about some alcoholic drinks being better or worse for you than others. But all types of alcohol increase the risk of cancer – as it’s the alcohol itself that causes damage, even in small amounts.
So the more you can cut down on alcohol the more you can reduce your risk of cancer.
Drinking less alcohol has lots of other health benefits, too. You can reduce your risk of accidents, high blood pressure and liver disease by cutting back.
Alcohol can damages our cells and this can stop cells repairing damage. Alcohol effects chemical signals which can make cells more likely to divide this in turn increases the chance of cancer to develop. Alcohol makes it easier for cell in our mouth and throat to absorb cancer causing chemicals.
There are many ways that alcohol can cause cancer. Some of the main ways are:
- Damage to cells. When we drink alcohol, our bodies turn it into a chemical, called acetaldehyde. Acetaldehyde can damage our cells and can also stop cells from repairing this damage.
- Changes to hormones. Alcohol can increase the levels of some hormones in our bodies such as oestrogen and insulin. Hormones are chemical messengers, and higher levels of oestrogen and insulin can make cells divide more often. This increases the chance that cancer will develop.
- Changes to cells in the mouth and throat. Alcohol can make it easier for cells in the mouth and throat to absorb harmful chemicals that cause damage.
Remember, it’s the alcohol itself that damages your body, even small amounts. It doesn’t matter whether you drink beer, wine or spirits. All types of alcohol can cause cancer.
There’s plenty of tricks that people claim ‘cure’ hangovers. But even if they work for your hangover, they don’t reverse the damage caused from drinking alcohol.
What types of cancer does alcohol cause?
Drinking alcohol causes 7 different types of cancer. This includes:
- Breast cancer and bowel cancer (two of the most common types)
- Mouth cancer
- Some types of throat cancer: oesophagus (food pipe), larynx (voice box) and pharynx (upper throat)
- Liver cancer
- Colon and Rectum
Stay tune for Part III in tomorrow’s article.
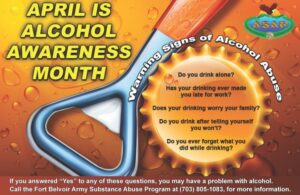

If yes to any of the questions listed in the first box above on the right side you may want to be checked out if you done know by now for your health!