Surgical Procedures for Vestibular Dysfunction When is surgery necessary?
When medical treatment isn’t effective in controlling vertigo and other symptoms caused by vestibular system dysfunction, surgery may be considered. The type of surgery performed depends upon each individual’s diagnosis and physical condition. Surgical procedures for peripheral vestibular disorders are either corrective or destructive. The goal of corrective surgery is to repair or stabilize inner ear function. The goal of destructive surgery is to stop the production of sensory information or prevent its transmission from the inner ear to the brain. The types of surgeries used if non-invasive treatments are not successful are possibly:
Labyrinthectomy:
A labyrinthectomy is a destructive procedure used for Ménière’s disease. The balance end organs are removed so that the brain no longer receives signals from the parts of the inner ear that sense gravity and motion changes. The hearing organ (cochlea) is also sacrificed with this procedure.
Vestibular nerve section:
A vestibular nerve section is a destructive procedure used for Ménière’s disease. The vestibular branch of the vestibulo-cochlear nerve is cut in one ear to stop the flow of balance information from that ear to the brain. The brain can then compensate for the loss by using only the opposite ear to maintain balance.
Chemical labyrinthectomy:
A chemical labyrinthectomy is also known as transtympanic or intratympanic treatment or gentamicin infusion. This is a destructive procedure used for Ménière’s disease. An antibiotic called gentamicin is introduced into the middle ear and absorbed via the round window. The drug destroys the vestibular hair cells so that they cannot send signals to the brain.
Endolymphatic sac decompression:
Endolymphatic sac decompression is a stabilizing procedure sometimes used for Ménière’s disease or secondary endolymphatic hydrops to relieve endolymphatic pressure in the cochlea and vestibular system. A variety of techniques exist. One method involves allowing the sac to decompress by removing the mastoid bone surrounding it. Other methods involve inserting a shunt (a tube or strip) into the endolymphatic sac so that, theoretically, excess fluid can drain out into the mastoid cavity or other location. The effectiveness of decompression techniques in controlling vertigo remains in doubt.
Oval or round window plugging:
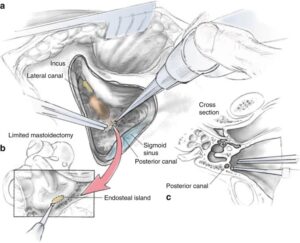
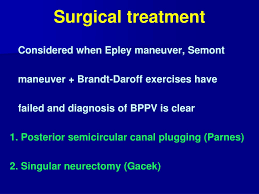
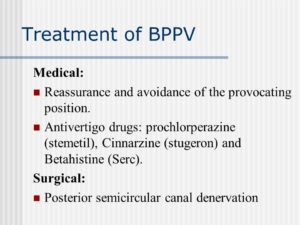
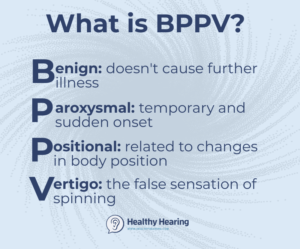
If the exercises described above are ineffective in controlling symptoms, symptoms have persisted for a year or longer, and the diagnosis is very clear, a surgical procedure called “posterior canal plugging” may be recommended. Canal plugging blocks most of the posterior canal’s function without affecting the functions of the other canals or parts of the ear. This procedure poses a substantial risk to hearing — ranging from 3-20%, but is effective in about 85-90% of individuals who have had no response to any other treatment (Shaia et al, 2006; Ahmed et al, 2012). The risk of the surgery to hearing derives from inadvertent breaking into the endolymphatic compartment while attempting to open the bony labyrinth with a drill. Sensibly, canal plugging for BPPV (note the first letter stands for “benign”) is rarely undertaken these days due to the risk to hearing.
Alternatives to plugging:
Singular nerve section is the main alternative. Dr Gacek (Syracuse, New York) has written extensively about singular nerve section (Gacek et al, 1995). Interestingly, Dr. Gacek is the only surgeon who has published any results with this procedure post 1993 (Leveque et al, 2007). Singular nerve section is very difficult because it can be hard to find the nerve.
Dr. Anthony (Houston, Texas), advocates laser assisted posterior canal plugging. It seems to us that these procedures, which require unusual amounts of surgical skill, have little advantage over a conventional canal plugging procedure. Oval or round window plugging is a stabilizing procedure sometimes used for repair of perilymph fistulas. Openings in the oval and/or round windows are patched with tissue taken from the external ear or from behind the ear so that perilymph fluid does not leak through the fistulas.
Pneumatic equalization (PE) tubes:
Pneumatic equalization (PE) is a stabilizing procedure sometimes used for treating perilymph fistulas. A tube is inserted through the tympanic membrane (eardrum) with one end in the ear canal and the other in the middle ear, to equalize the air pressure on the two sides of the eardrum.
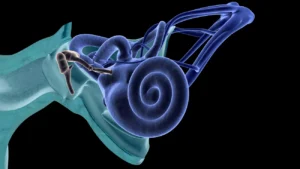
Canal partitioning (canal plugging):
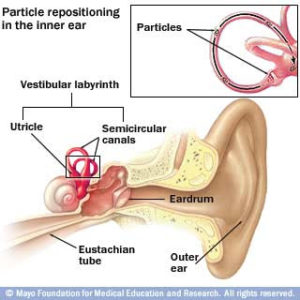
Canal partitioning is a stabilizing procedure sometimes used for treating BPPV or superior semicircular canal dehiscence. The problematic semicircular canal is partitioned or plugged with small bone chips and human fibrinogen glue to stop the movement of endolymph and foreign particles within the canal so that it no longer sends false signals to the brain.
Microvascular decompression:
Microvascular decompression is performed to relieve abnormal pressure of the vascular loop (blood vessel) on the vestibulo-cochlear nerve.
Stapedectomy:
Stapedectomy is a stabilizing procedure sometimes used for otosclerosis. It is accomplished by replacing the stapes bone with a prosthesis.
Acoustic neuroma (vestibular schwannoma):
This procedure involves the removal of a noncancerous tumor that grows from the tissue of the vestibular branch of the vestibulo-cochlear nerve.
Cholesteatoma removal:
This procedure involves the removal of a skin growth that starts in the middle ear and that can secrete enzymes that destroy bone and surrounding structures.
Ultrasound surgery:
Ultrasound is applied to the ear to destroy the balance end organs so that the brain no longer receives signals from the parts of the ear that sense gravity and motion changes. Cochlear dialysis Cochlear dialysis is a stabilizing procedure sometimes used to promote movement of excess fluid out of the inner ear by filling the scala tympani with a chemical solution.
Thanks to NYU Medical Hospital in Manhattan, NY you can Click here to download the “Surgery for Peripheral Vestibular Disorders” publication. – See more at: http://vestibular.org/understanding-vestibular-disorders/treatment/vestibular-surgery#sthash.GDeNWxjl.dpuf.
If you have this problem and need a great hospital than let us look at the ranking of hospitals:
Of all 180 hospitals in the New York, New York metropolitan area, the 53 listed below are the top-ranking. This metro area, also called NYC, includes Long Island, Westchester County, and northern New Jersey. I know if I had a problem that I could not get rid of immediately with a antibiotic simple cure I would next want to go to the best if my county’s hospital couldn’t remove the problem completely. So here through “US News and World Report” via the internet they show the following information on the best hospitals in NYC and Northern NJ: (Look below or to the next page)
These are their rankings on Columbia Presbyterian and NYU, NATIONALLY, in the following categories:
Starting with the best is Columbia Presbyterian in NY, for those in NY, as your #1 choice:
Adult Specialties
This hospital was among 144 facilities—roughly 3 percent of the 4,743 analyzed for the latest Best Hospitals rankings—to be ranked in even one of the 16 specialties.
COLUMBIA PRESBYTERIAN RATINGS:
| Nationally Ranked |
|
| High-Performing |
NYU HOSPITAL RATINGS:
- #50 in Cancer
- #11 in Cardiology & Heart Surgery
- #22 in Diabetes & Endocrinology
- #21 in Ear, Nose & Throat
- #26 in Gastroenterology & GI Surgery
- #8 in Geriatrics
- #38 in Nephrology
- #8 in Neurology & Neurosurgery************************ Impressive for neuro surgery of the ear.
- #4 in Orthopedics
- #33 in Pulmonology
- #9 in Rehabilitation
- #6 in Rheumatology
- #12 in Urology
Gynecology
| Rank in This Specialty | #NA |
| Overall Score in This Specialty | 66.8 / 100 |
For further checking of hospitals go to http://health.usnews.com/best-hospitals/area/ny/new-york-presbyterian-university-hospital-of-columbia-and-cornell-6210024 since hospitals do change yearly in their scores and this is the most recent.