Your blood carries oxygen and nutrients to all of the cells in your body. Blood cells also fight infection and control bleeding.
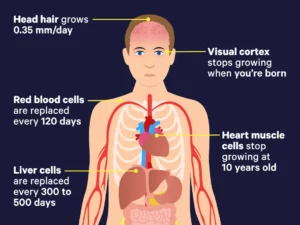
Most blood cells are made in your bone marrow. They are constantly being made and replaced. How long a blood cell lasts before being replaced is called its lifespan.
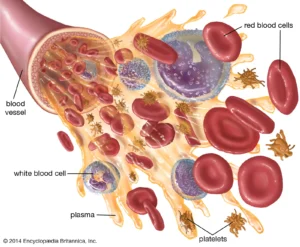
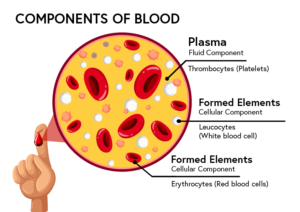
Your blood is made up of 4 parts: red blood cells, white blood cells, platelets, and plasma.
This information explains the different parts of your blood and their functions.
Your blood carries oxygen and nutrients to all of the cells in your body. Blood cells also fight infection and control bleeding.
Most blood cells are made in your bone marrow. They are constantly being made and replaced. How long a blood cell lasts before being replaced is called its lifespan.
Your blood is made up these 4 types of cells, lets review:
Parts of Your Blood
1-Red blood cells (erythrocytes)
Red blood cells carry oxygen from your lungs to your tissues. They also bring carbon dioxide back to your lungs.
Red blood cells make up almost half of your blood. The lifespan of a red blood cell is around 120 days.
2-White blood cells (leukocytes)
White blood cells fight infection and are an important part of your immune system. They make up a very small part of your total blood (less than 1%).
There are 3 types of white blood cells: I granulocytes, II monocytes, & III lymphocytes. Each type has an important role.
- I There are 3 types of granulocytes: A.Neutrophils help fight bacterial and fungal infections. B. Basophils are part of your body’s immune response/responses to allergens. Basophils are implicated in multiple human diseases including autoimmune disorders, inflammatory disorders, cancer and allergies and asthma. However, the contributions of basophils to the development of human disease states remain poorly defined. Their exact function isn’t well known. C.Eosinophils their main action is to help fight infections caused by parasites. A high number of eosinophils (eosinophilia) are often linked to a variety of disorders. A high eosinophil count may be due to: Adrenal gland deficiency. Also it could mean allergic disease, including hay fever.
- II Monocytes break down and remove foreign organisms and dying cells from your body. Main action against bacterial infection. They have subsets no Types (too much for this topic). Clevaland Clinic states “Monocytes are a type of white blood cell (leukocytes) that reside in your blood and tissues to find and destroy germs (viruses, bacteria, fungi and protozoa) and eliminate infected cells. Monocytes call on other white blood cells to help treat injury and prevent infection.
- III Lymphocytes make up your immune system. Lymphocytes are a type of white blood cell. They help your body’s immune system fight cancer and foreign viruses and bacteria. Your lymphocyte count can be taken during a normal blood test at your healthcare provider’s office. Lymphocyte levels vary depending on your age, race, sex, altitude and lifestyle.
Memorial Sloan Kettering Center in NYC states “White blood cells have a wide range of lifespans, from hours to years.”.
3-Platelets (thrombocytes)
Platelets are small parts of cells. Their main function is to control bleeding. They make up a very small part of your blood (less than 1%). The lifespan of platelets is about 9 to 12 days.
4-Plasma
Plasma is the pale-yellow liquid part of your blood that holds all of your blood cells. It makes up a little over half of your total blood.
Plasma helps move water, nutrients, minerals, medications, and hormones throughout your body. It also carries waste products to your kidneys. Then your kidneys filter out the waste products from your blood. Plasma is made up of water, protein, lipids (fats). It carries water, fat-soluble nutrients, and other substances to and from the different organs.
Resources
Johns Hopkins Medicine
www.hopkinsmedicine.org/health/wellness-and-prevention/facts-about-blood
This website has facts about blood, blood cells, and blood cell count.
American Red Cross
www.redcrossblood.org
The American Red Cross offers a variety of information about the different parts of blood and what blood cells do.
- Function of Blood and Blood Cells: www.redcrossblood.org/local-homepage/news/article/function-of-blood-cells.html
- Facts About Red Blood Cells: www.redcrossblood.org/donate-blood/dlp/red-blood-cells.html
- Facts About White Blood Cells: www.redcrossblood.org/donate-blood/dlp/white-cells-and-granulocytes.html
- Facts About Platelets: www.redcrossblood.org/donate-blood/dlp/platelet-information.html
- Facts About Plasma: www.redcrossblood.org/donate-blood/dlp/plasma-information.html
Stanford Children’s Health
www.stanfordchildrens.org
Stanford Children’s Health offers a variety of information about the different parts of blood and what blood cells do.
- Function of Blood and Blood Cells: www.stanfordchildrens.org/en/topic/default?id=overview-of-blood-and-blood-components-90-P02316
- Facts About Red Blood Cells: www.stanfordchildrens.org/en/topic/default?id=what-are-red-blood-cells-160-34
- Facts About White Blood Cells: www.stanfordchildrens.org/en/topic/default?id=what-are-white-blood-cells-160-35
- Facts About Platelets: www.stanfordchildrens.org/en/topic/default?id=what-are-platelets-160-36
- Facts About Plasma: www.stanfordchildrens.org/en/topic/default?id=what-is-plasma-160-37
 ZZXdcfvgbhnjmk,.
ZZXdcfvgbhnjmk,.