Part II Lung Cancer Awareness Month -Staging of NonSmall and Small Cell Lung Cancer and How Staging Works!
Understanding if and where lung cancer has spread (the stage) is important to determining what options are available for treatment. Imaging tests, biopsies and laboratory tests help to determine staging.
Non-Small Cell Lung Cancer
Non-small cell lung cancer is one of several cancers staged using the TNM system. The cancer is staged according to the size of the tumor (T), the extent to which the cancer has spread to the lymph nodes (N), and the extent to which the cancer has spread beyond the lymph nodes, or metastasis (M).
How Does The TNM Staging System Work?
The TNM staging system:
- Was created by merging the staging systems of the American Joint Committee on Cancer (AJCC) http://www.cancerstaging.org/ and the International Union Against Cancer (UICC) http://www.uicc.org/ in 1987
- Is one of the most commonly used cancer staging systems
- Standardizes cancer staging internationally
T is for Tumor
How big is the tumor? Where is it located? Has it spread to nearby tissue?
| TX | The primary tumor cannot be assessed, or the presence of a tumor was only proven by the finding of cancer cells in sputum or bronchial washings but not seen in imaging tests or bronchoscopy. |
| T0 | No evidence of a primary tumor. |
| Tis | “In situ” – cancer is only in the area where the tumor started and has not spread to nearby tissues. |
| T1 | The tumor is less than 3 cm (just slightly over 1 inch), has not spread to the membranes that surround the lungs (visceral pleura), and does not affect the air tunes (bronchi) that brand out on either side from the windpipe (trachea). |
| T1a | The tumor is less than 2 cm. |
| T1b | The tumor is larger than 2 cm but less than 3 cm. |
| T2 | The tumor is larger than 3 cm but less than 7 cm or involves the main air tubes (bronchus) that brand out from the windpipe (trachea) or the membranes that surround the lungs (visceral pleura). The tumor may partially block the airways but has not caused the entire lung to collapse (atelectasis) or to develop pneumonia). |
| T2a | The tumor is larger than 3 cm but less than or equal to 5 cm. |
| T2b | The tumor is larger than 5 cm but less than or equal to 7 cm. |
| T3 | The tumor is more than 7 cm or touches an area near the lung (such as the chest wall or diaphragm, or sac surrounding the heart (pericardium) or has grown into the main air tubes (bronchus) that brand out from the windpipe (trachea) but not the area where the windpipe divides or has caused one lunch to collapse (atelectasis) or pneumonia in an entire lung or there is a separate tumor(s) in the same lobe. |
| T4 | The tumor is of any size and has spread to the area between the lungs (mediastinum), heart, trachea, esophagus, backbone or the place where the windpipe (trachea) branches or there is a separate tumor(s) in a different lobe of the same lung. |
N is for Lymph Node
Has the cancer spread to the lymph nodes in and around the lungs? For more information on the lymph system and lymph nodes, see Lymph System
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No cancer found in lymph nodes. |
| N1 | Cancer has spread to lymph nodes within the lung or to the area where the air pipes (bronchus) that branch out from the windpipe enter the lung, but only on the same side of the lung as the tumor (ipsilateral). |
| N2 | Cancer has spread to lymph nodes near where the windpipe (trachea) branches into the left and right air tubes (bronchi) or near the area in the center of the lung (mediastinum) but only on the same side of the lung as the tumor. |
| N3 | Cancer has spread to lymph nodes found on the opposite side of the lung as the tumor (contralateral) or lymph nodes in the neck. |
M is for Metastasis
Has the cancer spread to other parts of the body?
| MX | Cancer spread cannot be assessed |
| M0 | Cancer has not spread. |
| M1 | Cancer has spread. |
| M1a | Cancer has spread: separate tumor(s) in a lobe in the opposite lung from the primary tumor (contralateral), or malignant nodules in the membrane that surround the lung (pleura) or malignant excess fluid (effusion) in the pleura or membrane that surround the hear (pericardium). |
| M1b | Cancer has spread to distant part of the body such as brain, kidney, bone. |
Stages
After the Tumor (T), Lymph Nodes (N) and Metastasis (M) have been determined, the cancer is then staged accordingly:
| Overall Stage | T | N | M |
|---|---|---|---|
| Stage 0 | Tis (in situ) | N0 | M0 |
| Stage IA | T1a, b | N0 | M0 |
| Stage IB | T2a | N0 | M0 |
| Stage IIA | T1a, b T2a T2b |
N1 N1 N0 |
M0 M0 M0 |
| Stage IIB | T2b T3 |
N1 N0 |
M0 M0 |
| Stage IIIA | T1, T2 T3 T4 |
N2, N1 N2, N0 N1 |
M0 M0 M0 |
| Stage IIIB | T4 Any T |
N2 N3 |
M0 M0 |
| Stage IV | Any T | Any N | M1a, b |
Small Cell Lung Cancer
Small cell lung cancer is most often staged as either limited-stage or extensive-stage.
Limited-Stage
Indicates that the cancer has not spread beyond one lung and the lymph nodes near that lung.
Extensive-Stage
The cancer is in both lungs or has spread to other areas of the body.
Source:
International Association for the Study of Lung Cancer. Goldstraw P, ed. Staging Handbook in Thoracic Oncology. Orange Park: Editorial Rx Press; 2009.
QUOTE FOR TUESDAY:
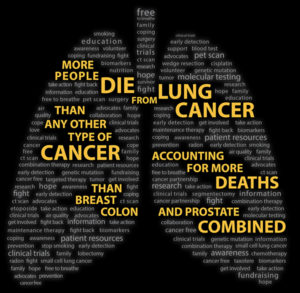
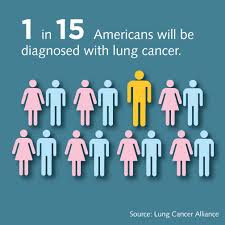
“Facts About Lung Cancer. LUNG CANCER is the leading cause of cancer death worldwide. AN ESTIMATED 238,340 PEOPLE will be diagnosed with lung cancer in 2023 in the U.S. 1 IN 16 PEOPLE will be diagnosed with lung cancer in their lifetime – 1 in 16 men, and 1 in 17 women.”
Lung Cancer Research Foundation (https://www.lungcancerresearchfoundation.org/lung-cancer-facts/)
Part I Lung Cancer Awareness Month
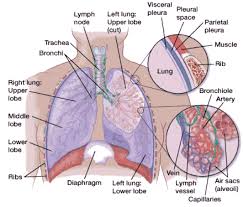
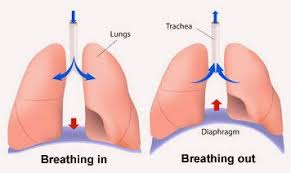
When you breathe in, air enters through your mouth and nose and goes into your lungs through the trachea (windpipe). The trachea divides into tubes called the bronchi (singular, bronchus), which enter the lungs and divide into smaller branches called the bronchioles. At the end of the bronchioles are tiny air sacs known as alveoli.
Many tiny blood vessels run through the alveoli. They absorb oxygen from the inhaled air into your bloodstream and pass carbon dioxide (a waste product from the body) into the alveoli. This is expelled from the body when you exhale. Taking in oxygen and getting rid of carbon dioxide are your lungs’ main functions.
A thin lining called the pleura surrounds the lungs. The pleura protects your lungs and helps them slide back and forth as they expand and contract during breathing. The space inside the chest that contains the lungs is called the pleural space (or pleural cavity).
Below the lungs, a thin, dome-shaped muscle called the diaphragm separates the chest from the abdomen. When you breathe, the diaphragm moves up and down, forcing air in and out of the lungs.
LUNG CANCER
There are 3 types of lungs cancer. The two most common types of lung cancer that exist are 1 non-small cell lung cancer (NSCLC), which is the most common, and 2 small cell lung cancer (SCLC), an aggressive cancer that occurs in just over 10 percent of all lung cancer cases.
The third group is 3 lung carcinoid tumors (also known as lung carcinoids) are a type of lung cancer, which is a cancer that starts in the lungs. Cancer starts when cells begin to grow out of control. Cells in nearly any part of the body can become cancer, and can spread to other areas of the body.
Lung carcinoid tumors are uncommon and tend to grow slower than other types of lung cancers. They are made up of special kinds of cells called neuroendocrine cells.
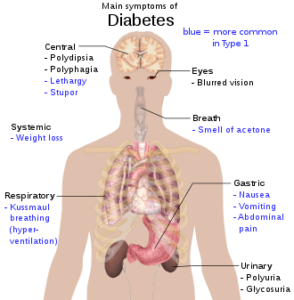
Lung Cancer Symptoms
Both major types of lung cancer have similar symptoms. These symptoms often include a cough that doesn’t go away and shortness of breath.
Sometimes lung cancer does not cause any signs or symptoms. It may be found during a chest X-ray done for another condition. Signs and symptoms may be caused by lung cancer or by other conditions. Check with your doctor if you have any of the following:
- Chest discomfort or pain
- A cough that doesn’t go away or gets worse over time
- Trouble breathing
- Wheezing
- Blood in sputum (mucus coughed up from the lungs)
- Hoarseness
- Loss of appetite
- Weight loss for no known reason
- Tiredness/lethargy
- Trouble swallowing
- Swelling in the face and/or veins in the neck
For both conditions, early detection through a low-dose computed topography (CT) scan is especially critical. Identifying lung cancer in its earliest stages even before you have symptoms can reduce the risk of death by 20 percent, according to recent studies.
Non-small cell lung Cancer (NSCLC)
Non-small cell lung cancer (NSCLC) is the most common type of cancer in lung tissues. Your risk of developing this disease increases if you are a longtime or former smoker, have been exposed to passive smoke, or have had environmental or occupational exposure to radon, asbestos, uranium, and other substances. The primary types of NSCLC are named for the type of cells found in the cancer:
- Squamous-cell carcinoma (also called epidermoid carcinoma)
- Adenocarcinoma
- Large-cell carcinoma
- Adenosquamous carcinoma
- Undifferentiatiated carcinoma
Small Cell Lung Cancer (SCLC)
In small cell lung cancer (SCLC), small cancerous cells arise in the airway, usually in a central location. This is an aggressive cancer that spreads quickly throughout the body through the blood and lymphatic (node) systems. Typically occurring in people who smoke or who used to smoke, SCLC accounts for just over 10 percent of all lung cancers.
QUOTE FOR MONDAY:
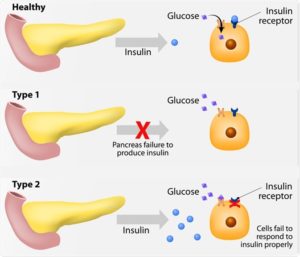
“In people with type 1 diabetes, the pancreas no longer makes insulin. The beta cells have been destroyed and they need insulin shots to use glucose from meals.
People with type 2 diabetes make insulin, but their bodies don’t respond well to it. Some people with type 2 diabetes need diabetes pills or insulin shots to help their bodies use glucose for energy.
Finding out you have diabetes can be overwhelming, but take a breath knowing you have a community to fall back on and the American Diabetes Association by your side to help you thrive.”.
American Diabetes Association (https://diabetes.org/)
Part VI Diabetes Awareness Month – Simply Understanding Insulin and how people can get Diabetes!
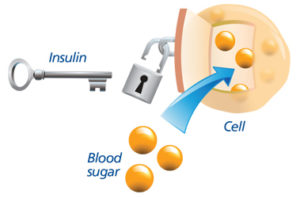
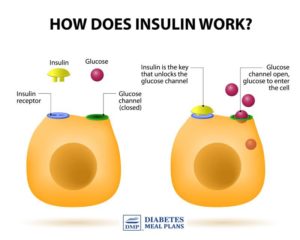
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use. Insulin helps keeps your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia). How it works; when the glucose gets in your body after digestion starting from eating or even if your not eating by mouth but through IV with Dextrose in it (a form of sugar) or just on a feeding tube via a nasogastric tube or gastric tube (PEG) with Dextrose or some form of sugar in it will put glucose in your blood. When you eat or drink, much of your food is broken down into a simple sugar called “glucose.” All 3 routes of getting nutrition can cause your glucose count in the bloodstream to go up, if some form of sugar is in the nutrition supply you get in your body for the cells in our bloodstream. Now glucose is food to our cells but the food has to get into the cells. For glucose to pass into our cells it needs a hormone to allow the glucose to pass in the cell to be the food for the cell. This is where Insulin comes into play! Insulin is released by the pancrease and put in our bloodstream to do one of its MAIN functions to allow glucose in the cell. For without insulin what happens is the glucose just will pile up outside of the blood cells and in time cause what we call Diabetes. Without glucose going into our cells through insulin allowing it to pass in the cells we would not have energy that helps us in doing our activities of daily living.
So in review, the amount of glucose in your bloodstream is tightly regulated by the hormone insulin. Insulin is always being released in small amounts by the pancreas but especially after eating and when digestion takes place releasing the broken down sugar to “glucose” being released into our blood. When the amount of glucose in your blood rises to a certain level, the pancreas will release more insulin to push more glucose into the cells.
Diabetes mellitus (sometimes called “sugar diabetes“) is a condition that occurs when the body can’t use glucose (a type of sugar) normally. Glucose is the main source of energy for the body’s cells. The levels of glucose in the blood are controlled by a hormone called insulin, which is made by the pancreas that it releases into the blood- stream when glucose level goes up allowing for it to be utilized by our body in allowing the glucose to transfer over the cell membranes into the cells as the main source of energy-a major form of nutrition for out cells to do its functions especially transfer oxygen throughout the body to keep our tissues healthy and alive. Without oxygen we would have tissue and cell starvation. Think in a diabetic when blood flow gets thick due to high glucose levels in the bloodstream making it difficult for the blood to move throughout our body to oxygenate our tissues the first place the body compensates to allow oxygenated blood by our cells to get to our vital organs like heart, lungs, brain and not areas far away from the body like feet. That is why you commonly hear of amputations of lower legs with uncontrolled or badly controlled diabetics (arms amputated is very, very rare due to diabetes, more its due to trauma.
People with diabetes either don’t make insulin or their body’s cells are resistant to insulin, leading to high levels of sugar circulating in the blood, called simply high blood sugar. By definition, diabetes is having a blood glucose level of 126 milligrams per deciliter (mg/dL) or more after an overnight fast (not eating anything).
So ending line without Insulin no glucose, a energy nutrition for our cells. we would not get glucose inside the cells. This as a ending result would cause cellular starvation of energy resulting into death in time (much sooner than other people without this problem) unless they take their insulin!
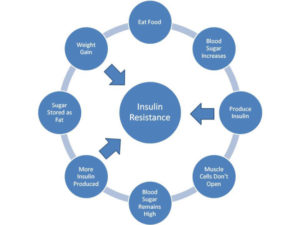
Another function of insulin is after our body uses all the glucose it needs at that time it needs to be stored somewhere. Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. To get the glucose level in therapeutic range for the body in time.
The 2 major groups of Diabetes occurs if someone has a problem with this role function of insulin resulting in one of the following:
Type 1 Diabetes occurs because the insulin-producing cells of the pancreas (called beta cells) are destroyed by the immune system. People with type 1 diabetes produce no insulin and must use insulin injections to control their blood sugar. This is most commonly seen in people under age 20 but may occur at any age.
Type 2 Diabetes is the most common form of diabetes, affecting almost 18 million Americans. While most of these cases can be prevented, it remains for adults the leading cause of diabetes-related complications such as blindness, non-traumatic amputations, and chronic kidney failure requiring dialysis. Type 2 diabetes usually occurs in people over age 40 who are overweight, but can occur in people who are not overweight as well.Sometimes referred to as “adult-onset diabetes,” type 2 diabetes has started to appear more often in children because of the rise in obesity in young people.
Sometimes referred to as “adult-onset diabetes,” type 2 diabetes has started to appear more often in children because of the rise in obesity in young people.
Some people can manage their type 2 diabetes by controlling their weight, watching their diet, and exercising regularly. Others may also need to take a pill that helps their body use insulin better, or take insulin injections.
Often, doctors are able to detect the likelihood of type 2 diabetes before the condition actually occurs. Commonly referred to as pre-diabetes, this condition occurs when a person’s blood sugar levels are higher than normal, but not high enough for a diagnosis of type 2 diabetes.
Know this diabetes can be hereditary as well.
Maybe you might want to get your glucose checked by your M.D. and make sure your insulin is functioning well for the side effects of uncontrolled diabetes are detrimental and could shorten your life!
QUOTE FOR THE WEEKEND:
“Diabetes is increasing at an alarming rate in the United States. According to the CDC’s (Centers for Disease Control) National Diabetes Statistics Report for 2022 cases of diabetes have risen to an estimated 37.3 million and one in five don’t know they have it.
The Cost of Diabetes
- In 2017, the total estimated cost of diagnosed diabetes in the U.S. was $327 billion.
- Total direct estimated costs of diagnosed diabetes increased from $188 billion in 2012 to $237 billion in 2017; total indirect costs increased from $73 billion to $90 billion in the same period (2017 dollars).
- Between 2012 and 2017, excess medical costs per person associated with diabetes increased from $8,417 to $9,601 (2017 dollars)
Remember without insulin, the body’s cells would go thru starvation, due to dehydration and destruction of body cells and tissues.
Diabetes was the seventh leading cause of death in the United States in 2017 based on the 83,564 death certificates in which diabetes was listed as the underlying cause of death.”
Diabetes Research (https://diabetesresearch.org/diabetes-statistics/)
Part V Diabetes Awareness Month-statistics, treatment, impact of cost & how to decrease it in the US!
Diabetes is still common in the United States. From 1980 through 2011, the number of Americans with diagnosed diabetes has more than tripled as of 2011 (from 5.6 million to 20.9 million).
Overall numbers the CDC reports in statistics up to 2020:
- Prevalence: In 2019, 37.3 million Americans, or 11.3% of the population, had diabetes.
- Nearly 1.9 million Americans have type 1 diabetes, including about 244,000 children and adolescents
- Diagnosed and undiagnosed: Of the 37.3 million adults with diabetes, 28.7 million were diagnosed, and 8.5 million were undiagnosed.
- Prevalence in seniors: The percentage of Americans age 65 and older remains high, at 29.2%, or 15.9 million seniors (diagnosed and undiagnosed).
- New cases: 1.4 million Americans are diagnosed with diabetes every year.
- Prediabetes: In 2019, 96 million Americans age 18 and older had prediabetes.
30.3 million – The number of people in the U.S. who had diabetes in 2022.
Do you know how much it is costing in our country? Its a combination of factors that has caused such and increase in the disease of Diabetes in the U.S. Factors:
-Look how much our population has increased with fast food companies pushing the unhealthy foods the sell in restaurants or food stores.
-Also people from other countries who permanently came into America becoming a citizen from 1980 to now and came in to the U.S. already eating poor OR picked up the bad habits of eating poor foods that the U.S. media pushes that is acceptable to enough by U.S. society (that is continues) and is adding to the diabetic population whether they came in the U.S. with it or got it when coming to live in America.
-Than people born in U.S. with family having a history of diabetes or worse parents who did not watch good eating habits when raising their children who got obese putting them at high risk for diabetes.
-Ending line, these factors massively increased making the number of Diabetic Americans 3x higher since 1980.
-Than another factor is the illegals with diabetes also adds to the number of diabetic people in America; for they are not left out and are treated in hospitals with citizens. If they come to an ER in the U.S. we treat them.
These factors all IMPACT an increase in the number of Diabetics in America!
Wake up America! We need to get this disease under better control! Diabetes increasing in the U.S. will not help disease overall in America!
That’s right. The metabolic condition is about as American as you can get, according to a national report card on diabetes by the Centers for Disease Control and Prevention 2011.
The report shows that nearly half of Americans have diabetes or prediabetes, which puts them at high risk for the condition. A good number of these folks haven’t been diagnosed and don’t even realize their predicament.
People with diabetes have too much sugar in their blood. If the disease isn’t controlled, they can wind up with heart disease, nerve damage, kidney problems, eye damage and other serious health problems.
That’s right. The metabolic condition is about as American as you can get, according to national report card on diabetes by the Centers for Disease Control and Prevention.
There are 2 types of Diabetes:
Type 1 diabetes was previously called insulin-dependent mellitus (IDDM) or juvenile-onset diabetes. This type of diabetes happens when the immune system ends up destroying beta cells in the body that come from our pancreas and they are the only cells in the human body that make the hormone INSULIN the regulates your glucose. Insulin allows glucose to transfer into the cells and tissues of our body to give them their energy to do their job in the body and nutrition to work properly=sugar-glucose. To live with this diabetes the person must have their insulin delivered by injection or a pump. This form of diabetes usually occurs in children or young adults but can occur at any age.
Type 2 diabetes was called non-insulin dependent diabetes mellitus (NIDDM) or adult-onset diabetes. In adults, type 2 diabetes accounts for about 90-95% of all diagnosed cases of diabetes. It usually begins as insulin resistance, a disease in which the cells do not use insulin properly due to the pancreas not making enough or the pancreas not secreting the correct form o of insulin to do its function. Ending line the insulin isn’t working properly. As the need for insulin rises, the pancreas gradually loses its ability to produce it.
Type 2 diabetes is associated with older age, OBESITY, family history of diabetes, history of gestational diabetes, impaired glucose metabolism, physical inactivity and race/ethnicity.
Gestational diabetes is a form of glucose intolerance diagnosed during pregnancy. Gestational diabetes occurs more frequently among African Americans, Hispanic/Latino Americans, and American Indians. It is also more common among obese women and women with a family history of diabetes. During pregnancy, gestational diabetes requires treatment to optimize maternal blood glucose levels to lessen the risk of complications in the infant.
Other types of diabetes result from; specific genetic conditions (such as maturity-onset diabetes of youth), surgery, medications, infections, pancreatic disease, and other illnesses. Such types of diabetes account for 1% to 5% of all diagnosed cases.
Treatment for Diabetes:
Diet, insulin, and oral medication to lower blood glucose levels are the foundation of diabetes treatment and management. Patient education and self-care practices are also important aspects of disease management that help people with diabetes lead normal lives or as normal as possible.
To survive, people with type 1 diabetes must have insulin delivered by injection or a pump.
Many people with type 2 diabetes can control their blood glucose by following a healthy meal plan and exercise program, losing excess weight, and taking oral medication.
Medications for each individual with diabetes will often change during the course of the disease. Some people with type 2 diabetes may also need insulin to control their blood glucose.
Self-management education or training is a key step in improving health outcomes and quality of life. It focuses on self-care behaviors, such as healthy eating, being active, and monitoring blood sugar.
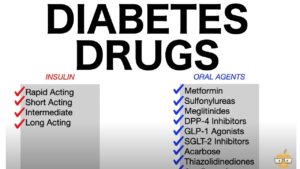
The medications used for diabetes could be that your endocrinologist would decide:
-Insulins-commonly in Type I DM but can be used if needed in Type II DM which the MD decides:
If you have type 1 diabetes, your body can’t make its own insulin. The goal of treatment is to replace the insulin that your pancreas can’t make.
Insulin is the most common type of medication used in type 1 diabetes treatment. There are more than 20 types sold in the United States.
It’s given as an infusion under the skin (with the help of an insulin pump) or as an injection.
There are multiple types of insulin. They vary based on how quickly they start working, how long they work, and whether they have a peak level of action.
The type of insulin you need depends on your body’s sensitivity to insulin and the severity of your insulin deficiency.
There are short acting, rapid acting, intermediate acting long acting, and combination insulins.
Also there is amylinomimetic. It’s an injectable medication that’s used before meals. It works by delaying the time your stomach takes to empty itself. It also reduces the secretion of the hormone glucagon after meals. These actions lower your blood sugar. Specifics are another topic in itself.
-Oral medications commonly used in type II diabetics; again specifics are another topic in itself.
If not doing treatment the diabetic will end up with severe complications to possibly death sooner in life than a compliant diabetic.
Pretty simple isn’t it but you have to the make a move quick if you haven’t yet! Take action and make changes if you need to!
How the cost of diabetes impacts America:
Diabetes is not only common and serious; it is also VERY COSTLY! This impacts medical insurance being so high since our population is so high in America. Let us take a look how:
The cost of treating diabetes is staggering. According to the American Diabetes Association, the annual cost of diabetes in medical expenses and lost productivity rose for $98 billion in 1997 to $132 billion in $2002 to $174 billion in 2007.
Two years ago in this post it stated one out of every 5 U.S. federal health care dollars is spent treating people with diabetes. The average yearly health care costs for a person without diabetes is 2,560 dollars; for a person with diabetes that figure soars to $11,744. Much of the human and financial costs can be avoided with proven diabetes prevention and management steps.
Now in 2022 the American Diabetes Association states “People with diagnosed diabetes incur average medical expenditures of $16,752 per year, of which about $9,601 is attributed to diabetes. On average, people with diagnosed diabetes have medical expenditures approximately 2.3 times higher than what expenditures would be in the absence of diabetes.” https://diabetes.org/about-us/statistics/cost-diabetes
Diabetes.org states now that “The estimated total economic cost of diagnosed diabetes in 2017 is $327 billion, a 26% increase from our previous estimate of $245 billion (in 2012 dollars).
The CDC states the following:
“The High Cost of Diabetes
Diabetes is the most expensive chronic condition in our nation.15,16
- $1 out of every $4 in US health care costs is spent on caring for people with diabetes.15
- $237 billion‡(c) is spent each year on direct medical costs and another $90 billion‡(c) on reduced productivity.15
- The total economic cost of diabetes rose 60% from 2007 to 2017.15
- 61% of diabetes costs are for people 65 years or older, which is mainly paid by Medicare.15
- 48% to 64% of lifetime medical costs for a person with diabetes are for complications related to diabetes, such as heart disease and stroke.17″
So think if we decreased diabetes and many other diseases diabetes can cause how much we in America would decrease medical costs in America and help our economy drastically!!
If you agree be healthy and than those with diabetes (DM) being compliant will help you as an individual but compliant diabetics in numerous quantity will also help the economy. Even helping economy more would be people without DM preventing DM from ever occuring. Both compliant diabetics and people living a healthy to prevent diabetes would drastically help our economy with decreasing the medical costs for diabetes.
QUOTE FOR FRIDAY:
“Diabetes is a serious, long-term condition with a major impact on the lives and well-being of individuals, families, and societies worldwide. The global diabetes prevalence in 2019 is estimated to be 9.3% (463 million people), rising to 10.2% (578 million) by 2030 and 10.9% (700 million) by 2045 [1]. Population aging is also increasing dramatically throughout the world, especially in developing countries, creating pressures on the health system as well as social security services and policies. Nowadays, many people are familiar with type 1 or type 2 diabetes mellitus, however, there is another form of diabetes that has just recently been identified, known as type 3 diabetes (T3DM). This lesser-known type manifests as insulin resistance within the brain and has major potential to impact neurocognition and contributes to the etiology of Alzheimer’s disease [AD]. AD has already been identified as the sixth leading cause of death in the United States, and the fifth leading cause of mortality in people 65 and older.”
National Library of Medicine – NIH (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246646/)
Part III Diabetes Awareness Month – Alzheimer’s Disease considered by some as Brain Diabetes!
It’s Alzheimer’s Disease and Dementia Care Education Month.
At one time Alzheimer’s disease was a disease considered with unknown etiology (or cause). Today it is considered different in the eyes of many in the medical profession. By a Dr. Mercola a physician who founded Mercola.com (Mercola.com is now the world’s top natural health resource site, with over 1.5 million subscribers.) feels this about Alzheimer’s disease: “The cause of the debilitating, and fatal, brain disease Alzheimer’s is conventionally said to be a mystery.”
While we know that certain diseases, like type 2 diabetes, are definitively connected to the foods you eat, Alzheimer’s is generally thought to strike without warning or reason.
That is, until recently.
Now, a growing body of research suggests there may be a powerful connection between the foods you eat and your risk of Alzheimer’s disease and dementia, via similar pathways that cause type 2 diabetes. Some have even re-named Alzheimer’s as “type 3 diabetes.””
Can You Eat Your Way to Alzheimer’s?
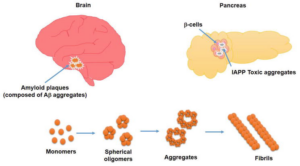
In a recent animal study, researchers from Brown University in Providence, Rhode Island were able to induce many of the characteristic brain changes seen with Alzheimer’s disease (disorientation, confusion, inability to learn and remember) by interfering with insulin signaling in their brains.
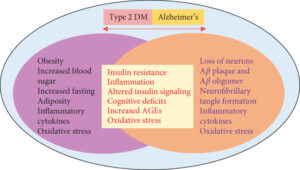
Know that faulty insulin (and leptin, another hormone) signaling is an underlying cause for insulin resistance, which, of course, typically leads to type 2 diabetes. However, while insulin is usually associated with its role in keeping your blood sugar levels in a healthy range, it also plays a role in brain signaling. When researchers disrupted the proper signaling of insulin in the brain, it resulted in dementia.
What does this have to do with your diet? Let us go back to one of my articles on diabetes this week and how it impacts your diet. It states “The foods we eat that contain starches, carbohydrates, calories are made up of sugar. When food reaches our stomach in time digestion starts to take place where these foods are broken down in the stomach into individual or complex sugar molecules ( glucose being one of the most common and important ones). The glucose then passes from our stomach into our bloodstream when it reaches the liver 60 to 80 % of the glucose gets stored in that organ turning glucose into inactive glucose that’s converted to glycogen. The purpose for glycogen is when our glucose is low and our body needing energy we have this extra stored sugar, glycogen, to rely on. This is done by the liver which allows the sugar to be stored and released back into the bloodstream if we need it=energy, since nothing is in our stomach at that time, in that case scenario). When glucose=an active sugar, it is our energy for our cells and tissues and is a sugar ready to be utilized by the body where it is needed, by many organs. Think of a car for one moment, and what makes it run? That would be gas/fuel for it to function. The same principle with glucose in your bloodstream=fuel for the human body so we can function, for without it we wouldn’t survive. That is the problem with a person that has diabetes. They eat, they break the food down, the glucose gets in the blood but the glucose fuel can’t be used due to lack of or NO insulin at all. Insulin allows glucose to pass into our cells and tissues to be used as energy/fuel for the body parts to work. Glucose is used as the principle source of energy (It is used by the brain for energy, the muscles for both energy and some storage, liver for more glucose storage=that is where glucose is converted to glycogen, and even stored in fat tissue using it for triglyceride production). Glucose does get sent to other organs for more storage, as well. Insulin plays that vital role in allowing glucose to be distributed throughout the body. Without insulin the glucose has nowhere to go.”
So how does this impact your brain thinking?
“This new focus on the Alzheimer’s/Diabetes/Insulin connection follows a growing recognition of insulin’s role in the brain. Until recently, the hormone was typecast as a regulator of blood sugar, giving the cue for muscles, liver and fat cells to extract sugar from the blood and either use it for energy or store it as fat. We now know that it is also a master multitasker: it helps neurons, particularly in the hippocampus and frontal lobe, take up glucose for energy, and it also regulates neurotransmitters, like acetylcholine, which are crucial for memory and learning.” What is effected with Alzheimer’s disease? Your memory and learning, So your diet plays a big role in Alzheimer’s disease.”
Over-consumption of sugars and grains is what ultimately causes your body to be incapable of “hearing” the proper signals from insulin and leptin, leaving you insulin resistant in both body and brain. Alzheimer’s disease was tentatively dubbed “type 3 diabetes” in early 2005 when researchers learned that the pancreas is not the only organ that produces insulin. Your brain also produces insulin, and this brain insulin is necessary for the survival of your brain cells.
If You Have Diabetes, Your Risk of Alzheimer’s Increases Dramatically
Diabetes is linked to a 65 percent increased risk of developing Alzheimer’s, which may be due, in part, because insulin resistance and/or diabetes appear to accelerate the development of plaque in your brain, which is a hallmark of Alzheimer’s. Separate research has found that impaired insulin response was associated with a 30 percent higher risk of Alzheimer’s disease, and overall dementia and cognitive risks were associated with high fasting serum insulin, insulin resistance, impaired insulin secretion and glucose intolerance.
A drop in insulin production in your brain may contribute to the degeneration of your brain cells, mainly by depriving them of glucose, and studies have found that people with lower levels of insulin and insulin receptors in their brain often have Alzheimer’s disease (people with type 2 diabetes often wind up with low levels of insulin in their brains as well). As explained in New Scientist, which highlighted this latest research:
What’s more, it encourages the process through which neurons change shape, make new connections and strengthen others. And it is important for the function and growth of blood vessels, which supply the brain with oxygen and glucose.
As a result, reducing the level of insulin in the brain can immediately impair cognition. Spatial memory, in particular, seems to suffer when you block insulin uptake in the hippocampus… Conversely, a boost of insulin seems to improve its functioning.
When people frequently gorge on fatty, sugary food, their insulin spikes repeatedly until it sticks at a high level. Muscle, liver and fat cells then stop responding to the hormone, meaning they don’t mop up glucose and fat in the blood. As a result, the pancreas desperately works overtime to make more insulin to control the glucose – and levels of the two molecules skyrocket.
The pancreas can’t keep up with the demand indefinitely, however, and as time passes people with type 2 diabetes often end up with abnormally low levels of insulin.”

 =
=