Early detection of lung cancer can save lives!
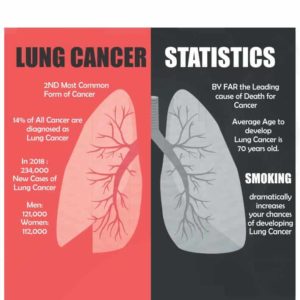
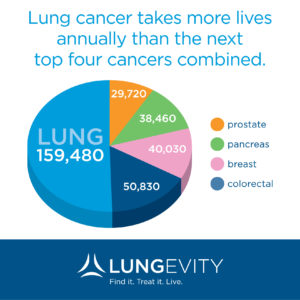
You may be surprised to learn that the most deadly cancer among both men and women in the United States isn’t breast cancer: It’s lung cancer.
Although the rate of new lung cancer cases has dropped in recent years along with the smoking rate, lung cancer still accounts for more deaths than any other cancer in both men and women, according to the American Cancer Society.
So even though you’ll probably never see professional athletes sporting pearl-colored gloves and shoes (pearl is the color of the lung cancer ribbon) to raise awareness, it’s important to learn about the disease: who is at risk — not just people who smoke tobacco — how it’s treated and why early detection is the best defense.
Here, Mary Jo Fidler, MD, a medical oncologist at Rush University Medical Center, discusses five things everyone should know about lung cancer.
1. It’s often caused by a combination of factors.
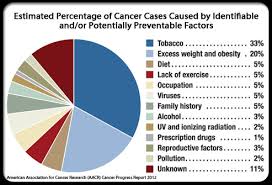
“It’s natural to associate lung cancer with cigarette smoking,” Fidler says. “Although it’s true that smoking is responsible for 80 percent of all lung cancer cases, lung cancer among people who have never smoked is the sixth leading cause of cancer death worldwide.”
These are some of the leading causes of lung cancer among nonsmokers:
- Exposure to radon gas released from soil and building materials
- Exposure to asbestos, diesel exhaust and/or industrial chemicals
- Exposure to secondhand smoke (the U.S. Department of Health and Human Services says secondhand smoke increases a nonsmoker’s lung cancer risk by as much as 20 to 30 percent)
- Air pollution
And while any of these factors can cause lung cancer on its own, the disease is often the result of interacting factors.
For instance, according to the National Institutes of Health, there is a greater risk for lung cancer when smokers are also exposed to radon gas. And research studies have shown that the combination of smoking and asbestos exposure greatly increases a person’s risk of developing lung cancer vs. both nonsmoking asbestos workers and smokers who are not exposed to asbestos.
Occupational exposures — including asbestos, uranium and coke (a type of fuel used in smelters, blast furnaces and foundries) — can also increase a person’s risk of dying from their lung cancer, according to another study.
2. Genes may play a role in lung cancer risk.
Scientists have discovered that another culprit may be responsible for some nonsmokers getting lung cancer: genetics.
A study published in the journal Nature Genetics identified three genetic variations — two on chromosome 6 and one on chromosome 10 — that are associated with increased lung cancer risk in Asian women who have never smoked.
Findings have shown that the risk of lung cancer among people who never smoked, especially Asian women, may be associated with specific genetic characteristics that distinguish it from lung cancer in smokers.
Another study, published in Cancer, found that a variant in the NFKB1 gene was associated with a 21 to 44 percent reduced risk of lung cancer. Because a protein produced in part of the NFKB1 gene is known to play a significant role in inflammation and immunity by regulating gene expression, cell death and cell production, the study suggests that inflammation and immune response may be associated with lung cancer risk.
Further research is needed, however, to determine whether there’s a cause and effect relationship between this variant in the NFKB1 gene and lung cancer. Future studies may also shed more light on the exact role inflammation plays in lung cancer risk.
3. If you’re at high risk, CT scans are an effective screening tool.
As with other cancers, the key to surviving lung cancer is catching it in the earliest stages, when it’s most treatable.
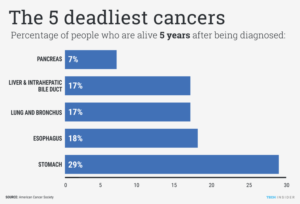
The five-year survival rate for people whose cancers are diagnosed when they’re still localized — meaning they haven’t yet spread to the lymph node drainage system or other areas of the body — can be as high as 80 to 90 percent; the survival rate plummets to 2 percent if the diagnosis happens after the cancer has spread to other body parts.
Unfortunately, because symptoms (including persistent cough or coughing up blood, unexplained weight loss, persistent chest pain and shortness of breath) don’t usually appear until the later stages, lung cancer is tough to diagnose early.
Low-dose spiral computed tomography (CT) has proven to reduce lung cancer deaths in patients at high risk for lung cancer. In fact, the National Lung Screening Trial found a 20 percent reduction in deaths from lung cancer among current or former heavy smokers who were screened with low-dose spiral CT (versus those screened by chest X-ray).
However, because the scans can also yield false positive results — by mistaking scar tissue or benign lumps for cancer — they’re recommended only for people at high-risk, for whom the benefits of early detection outweigh the risks of potential false positives and repeated exposure from the scans.
Lung cancer screening is recommended for people who meet these criteria:
- Are between the ages of 55 and 77 (for Medicare coverage) and 55 and 80 (for commercial insurance coverage)
- Have at least a 30 pack-year smoking history (an average of one pack a day for 30 or more years)
- Are in good health and have no signs of lung cancer (weight loss or coughing up blood)
- Have not had a chest CT in the past year.
“Talk to your doctor if you’re in this high-risk group,” says Fidler. “The best evidence we have available tells us that while CT scanning isn’t right for everyone, for those at high risk it does prevent lung cancer deaths by enabling earlier diagnoses.”
We have had a historically huge amount of FDA approvals in a relatively short amount of time for lung cancer therapies, which is good reason for optimism.
4. Some tumors can be removed minimally invasively.
Tumors that are caught in the early stages can often be surgically removed, giving patients a good chance of being cancer-free.
The standard procedure to remove the lobe of the lung in which the tumor is located, known as a lobectomy, typically requires a six-inch incision in the chest through which the ribsare spread apart.
But at a handful of medical centers, including Rush, roughly 80 percent of lobectomies can be done using a minimally invasive approach.
Video-assisted thoracoscopic surgery (VATS) lobectomies are performed through small incisions (and without spreading the rib cage) using a tiny video camera and specialized surgical instruments. There are many benefits to a VATS lobectomy vs. open surgery — including less pain and fewer complications after surgery, less time in the hospital and a speedier recovery — and the results are comparable, making it a good option for many tumors.
5. Newer treatments pack a targeted punch.
Research has yielded a wealth of information about how lung cancer cells change and grow, enabling scientists to develop drugs to specifically address those changes.
These “targeted” drug therapies, used alone or in combination with chemotherapy, are typically less toxic and have fewer side effects than chemotherapy because they zero in on specific genes or proteins more often found in cancer cells then in healthy tissue.
These are some of the targeted therapies currently available for lung cancer
- Monoclonal antibodies (bevacizumab, ramucirumab)
- EGFR inhibitors (erlotinib, afatinib, gefitinib)
- Osimertinib, an EGFR inhibitor that also targets cells with the T790M mutation
- Necitumumab, an EGRF inhibitor for squamous cell non-small cell lung cancer
- Drugs that target the ALK gene (crizotinib, ceritinib, alectinib)