
Treats: Warn children not to eat any treats before an adult has carefully examined them for evidence of tampering.
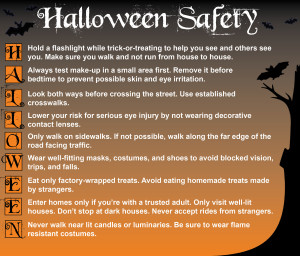
Flame Resistant Costumes: When purchasing a costume, masks, beards, and wigs, look for the label Flame Resistant. Although this label does not mean these items won’t catch fire, it does indicate the items will resist burning and should extinguish quickly once removed from the ignition source. To minimize the risk of contact with candles or other sources of ignition, avoid costumes made with flimsy materials and outfits with big, baggy sleeves or billowing skirts.
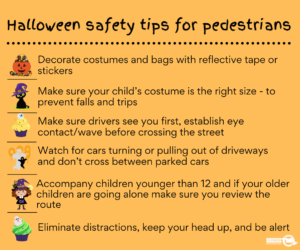
Costume Designs: Purchase or make costumes that are light and bright enough to be clearly visible to motorists.
For greater visibility during dusk and darkness, decorate or trim costumes with reflective tape that will glow in the beam of a car’s headlights.
Bags or sacks should also be light colored or decorated with reflective tape. Reflective tape is usually available in hardware, bicycle, and sporting goods stores.
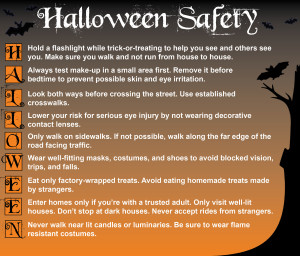
To easily see and be seen, children should also carry flashlights.
Costumes should be short enough to prevent children from tripping and falling.
Children should wear well-fitting, sturdy shoes . Mother’ s high heels are not a good idea for safe walking.
Hats and scarfs should be tied securely to prevent them from slipping over children’s eyes.
Apply a natural mask of cosmetics rather than have a child wear a loose-fitting mask that might restrict breathing or obscure vision. If a mask is used, however, make sure it fits securely and has eyeholes large enough to allow full vision. Swords, knives, and similar costume accessories should be of soft and flexible material.
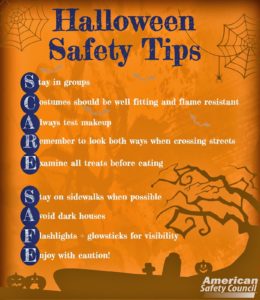
Pedestrian Safety: Young children should always be accompanied by an adult or an older, responsible child. All children should WALK, not run from house to house and use the sidewalk if available, rather than walk in the street.
Children should be cautioned against running out from between parked cars, or across lawns and yards where ornaments, furniture, or clotheslines present dangers.
Choosing Safe Houses: Children should go only to homes where the residents are known and have outside lights on as a sign of welcome.
Children should not enter homes or apartments unless they are accompanied by an adult.
People expecting trick-or-treaters should remove anything that could be an obstacle from lawns, steps and porches.
Candlelit jack-o’-lanterns should be kept away from landings and doorsteps where costumes could brush against the flame. Indoor jack-o’-lanterns should be kept away from curtains, decorations, and other furnishings that could be ignited.
Even though it’s not an official holiday, Halloween is much beloved by children and adults alike. What could be more fun than trick-or-treating, apple bobbing, or costume parties?
To make sure treats are safe for children, follow these simple steps:
Snacking: Children shouldn’t snack on treats from their goody bags while they’re out trick-or-treating. Give them a light meal or snack before they head out – don’t send them out on an empty stomach. Urge them to wait until they get home and let you inspect their loot before they eat any of it.
Safe treats: Tell children not to accept – and especially not to eat – anything that isn’t commercially wrapped. Inspect commercially wrapped treats for signs of tampering, such as an unusual appearance or discoloration, tiny pinholes, or tears in wrappers. Throw away anything that looks suspicious.
Food Allergies: If your child has a food allergy, check the label to ensure the allergen isn’t present. Do not allow the child to eat any home-baked goods he or she may have received.
Choking hazards: If you have very young children, be sure to remove any choking hazards such as gum, peanuts, hard candies, or small toys.
Bobbing for apples is an all-time favorite Halloween game. Here are a couple of ways to say “boo” to bacteria that can cause foodborne illness. Reduce the number of bacteria that might be present on apples and other raw fruits and vegetables by thoroughly rinsing them under cool running water. As an added precaution, use a produce brush to remove surface dirt.
Try this new spin on apple bobbing from FightBAC.org: Cut out lots of apples from red construction paper. On each apple, write activities for kids, such as “do 5 jumping jacks.” Place a paper clip on each apple and put them in a large basket. Tie a magnet to a string. Let the children take turns “bobbing” with their magnet and doing the activity written on their apple. Give children a fresh apple for participating.
If your idea of Halloween fun is a party at home, don’t forget these tips:
- Beware of spooky cider! Unpasteurized juice or cider can contain harmful bacteria such as Salmonella. To stay safe, always serve pasteurized products at your parties.
- No matter how tempting, don’t taste raw cookie dough or cake batter that contain uncooked eggs.
- “Scare” bacteria away by keeping all perishable foods chilled until serving time. These include finger sandwiches, cheese platters, fruit or tossed salads, cold pasta dishes with meat, poultry, or seafood, and cream pies or cakes with whipped-cream and cream-cheese frostings.
Bacteria will creep up on you if you let foods sit out too long. Don’t leave perishable goodies out of the fridge for more than two hours (1 hour in temperatures above 90°F).