 AFIB Symptoms.
AFIB Symptoms.
 12Lead EKG with AFIB.
12Lead EKG with AFIB.
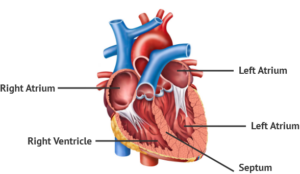
Working of the heart:
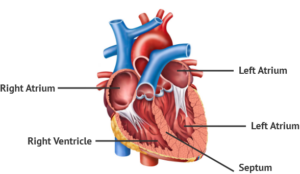
The anatomy to know in this discussion it you have 4 chambers and flow the blood through the heart. Below is a picture of the heart showing vessels mainly carbon dioxide in blood=color blue & oxygenated vessels=color red.

 The Ventricles of the HEART
The Ventricles of the HEART
Our blood needs to be oxygenated and when oxygen is used up we have more de-oxygenated or high carbon dioxide (CO2) levels in the red blood cells in the blood stream that go to our lungs for oxygen from the right side of our heart, which is used up oxygen blood in our red blood cells to more carbon dioxide in the cell than oxygen. So now those cells have to get replaced with oxygen and to that blood reaches the lungs from the right side of the heart pumping the blood, as its motility, to get to the lungs for more oxygen.
The RBC’s filled with more carbon dioxide are sent to the right side of the heart; first the right atrium to the right ventricle to the pulmonary artery to the lungs for more oxygen.
When we breath a oxygen / carbon dioxide process takes place at the bottom of the lungs. We send oxygen down to our lungs and send out CO2 from our body to replace it with more oxygen. This is how it works; when we inhale we send oxygen down to the lungs to replace the CO2 in our red blood cells (RBC’s). We have to get rid of CO2 for replacement with oxygen. When we exhale we send that gas, carbon dioxide, out of our blood stream and upon inhaling we send oxygen down to the lungs to replace the CO2 in our red blood cells (RBC’s). That carbon dioxide blood in our RBC’s get sent out of the RBC’s leaving the membrane of the cell going into the lungs where a gas exchange takes place replaced with oxygen passing the RBC membrane into the RBC that’s in our blood at the bottom of the lungs that we get when we breath. Those RBC’s that are now oxygenated are sent in the bloodstream to the left side of the heart where the heart pumps sending that oxygenated blood to all body tissues/organs to stay alive from the left atrium to left ventricle and sent out the aorta to all body parts.
When we do the process of breathing it is what allows the exchange of gases to take place at the RBC’s. Without oxygen we would have RBC starvation and we would be dead unless we where on a ventilator doing our breathing process.
Knowing this also know we have areas of the heart that play an effect with cardiac impulses from our natural pacemaker of the heart SA node in the right atrium that sends cardiac impulsed all the way down the heart to send messages to the heart in doing beating and function that is not discussed in this since it would be a chapters. Know this part the SA node is effected which when its now we are probably in a rhythm NSR normal sinus rhythm but when the SA node doesn’t work other areas in the atrium take over causing other rhythms and one could be atrial fibrillation or not.
So now with a quick overview of the anatomy of the 4 chambers of your heart and the process of breathing for 02 and CO2 and a quick touch of the firing system at the SA node lets go into atrial fibrillation also known as afib.
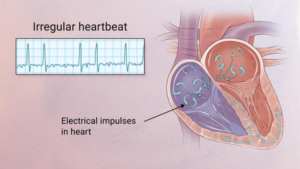
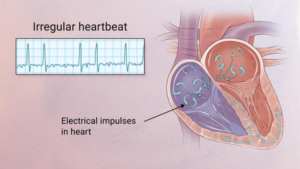
Understand in atrial fibrillation you show a line that squabbly with a pointed line. The squabble line is
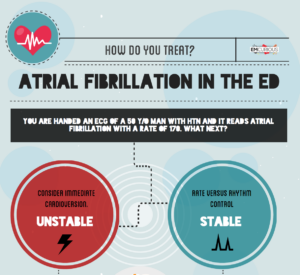
To easily identify atrial fibrillation with RVR, it is vital to understand the working of the heart.
The atrium or atria (plural) is the upper chamber of the heart, the heart has 2 atrium. Now, in size compared to atriums you have the lower 2 chambers known as the ventricles and they are larger.
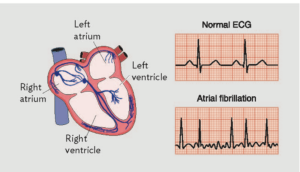
The atria function by gathering blood as it flows into the heart and shrinking to forward the blood into the ventricles. At the very moment, the ventricle must shrink to forward the blood to all parts of the body. This rhythm of blood flow creates a heart signature voice referred to as the Sinus rhythm. It is important that the sinus rhythm is synchronized so that the atrium does not send blood into the ventricle out of cue. To achieve this, an electric signal is generated to ensure the atrium contracts. When this signal short circuits (bypasses) the atrium, atrial fibrillation with RVR occurs, and the atrium is seen to vibrate just like jelly on a flat surface (see the second picture posted above to see the rhythm).
Atrial fib with RVR refers to atrial fibrillation with rapid ventricular rate. Usually the heart is like clockwork, the top (collecting) chambers beat then the bottom (main pumping) chambers sense this and also beat, and so on, in a nice regular fashion just like a clock ticking second after second. Usually the heart beats at about 60-80 beats per minute.
What is Atrial Fibrillation and RVR:
In atrial fibrillation the top chamber basically goes crazy often firing off over 400 beats per minute! Atrial fibrillation with RVR (Rapid Ventricular Response) is a heart condition caused by irregular electrical activity that results in irregular contractions of the 2 top heart chambers fibrillating. This means the heart (atriums), shakes with a rapid tremulous movement or makes fine irregular twitching movements, generally referred to as fibrillating in the upper chambers of the heart (atriums) causing little control in the heart output of blood by the heart making the lower chambers called the ventricles to take over. Know when the atrial chambers can’t work the ventricles take over but know this they are pumping a slower than 400 beats a minute and could range from 100 and up to 200 if not controlled.
These bottom chambers don’t allow all those impulses through but it does let every second or third one through. This can give a heart rate of 100-180 beats per minute at rest, still too many beats, known as Afib with RVR, leading to symptoms and problems with heart function. Afib does not necessarily lead to Afib with RVR however, Afib can be rate controlled, sometimes naturally, sometimes using medications and sometimes requiring procedures.
In most people with AFib although symptoms can sometimes be unpleasant it is generally not harmful as long as the afib is controlled, meaning the heart in the afib rhythm with the pulse under 100. The main concern is stroke, but that can be treated with the use of blood thinning medications in people at risk. In Afib with RVR, basically the heart is beating too fast. Of course palpitations are the most common symptom. Other symptoms of AFib with RVR may include dizziness, lack of energy, exercise intolerance and shortness of breath. If Afib with RVR goes on for too long then this may result in heart failure and of course worsening of existing heart failure. Control of the heart rate in patients with Afib with RVR often causes these symptoms to improve, again meaning the HR is under 100 with the heart rhythm in afib.
A major indication of atrial fibrillation with RVR is a very rapid heartbeat rate, although some patients are known to have the condition without showing symptoms. Atrial fibrillation with RVR may occur when cardiac muscle cells overcome their intrinsic pacemaker’s signals and fire rapidly differently from their normal pattern spreading the abnormal activity to the ventricles. The rapid heart rate can strain the heart, developing a situation referred to as Tachycardia (meaning a pulse greater than 100). Atrial fibrillation with RVR can be detected from the various symptoms though it is important to remember that some patients have experienced the condition without symptoms.
Always remember the human body is like a car in the following:
The CAR’s heart is the engine! The CAR’s lungs are the transmission! One can’t live without the other or the car will die! Without these part’s the car won’t start to run if the engine is damaged completely and it won’t be able to allow the car to slow down or speed up via the transmission!
The BODY’s engine is the heart! The BODY’s transmission is the LUNGS. One can’t live without the other or the body will die! Without them we will have no air exchange process and the tissues or organs or our body don’t get their food call oxygen and removing the toxic carbon dioxide!



 The Ventricles of the HEART
The Ventricles of the HEART