QUOTE FOR MONDAY:
“Labor Day 2024 will occur on Monday, September 2. Labor Day pays tribute to the contributions and achievements of American workers and is traditionally observed on the first Monday in September. It was created by the labor movement in the late 19th century and became a federal holiday in 1894. Labor Day weekend also symbolizes the end of summer for many Americans and is celebrated with parties, street parades and athletic events.
Labor Day, an annual celebration of workers and their achievements, originated during one of American labor history’s most dismal chapters.
In the late 1800s, at the height of the Industrial Revolution in the United States, the average American worked 12-hour days and seven-day weeks in order to eke out a basic living. Despite restrictions in some states, children as young as 5 or 6 toiled in mills, factories and mines across the country, earning a fraction of their adult counterparts’ wages.”
History (https://www.history.com/topics/holidays/labor-day-1#why-do-we-celebrate-labor-day)
Happy Labor Day to All and to those off enjoy the holiday and to those not thank you for working the holiday!
QUOTE FOR THE WEEKEND:
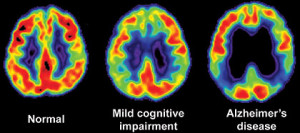
“Opioids are a class of substances that inhibit the transmission of painful stimuli [1]. They are characterized by a strong analgesic effect. Opioids may be legally prescribed in the form of opiates such as codeine, morphine, semisynthetic opioids such as oxycodone, synthetic opioids such as fentanyl [2], and there are also illegal forms such as heroin
In the United States, from 1999 to 2019, opioid overdose, either regularly prescribed or illegally acquired, was the cause of death for nearly 500,000 people. In addition to this pronounced mortality burden that has increased gradually over time, opioid overdose has significant morbidity with severe risks and side effects. As a result, opioid misuse is a cause for concern and is considered an epidemic”
National Library of Medicine – NIH (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9517221/)
Opioid Misuse Prevention Day is August 31st
Opioid addiction remains one of the primary public health crises in the nation. In order to fight it, everyone needs to do their part. The medical community is taking steps to address the frequency with which they prescribe opioid-based pain medications. Law enforcement has stepped up their efforts to reduce the influx of synthetic opioids such as fentanyl and carfentanyl. Unison Health has increased its capacity to treat substance abuse disorders through its Sub-Acute Detox facility and Recovery Housing.
PREVENT MISUSE IN THE FIRST PLACE:
One of the best ways to prevent you or the people around you from misusing opioids is to not have any around in the first place! If you’ve been prescribed opioid-based prescription pain medications in the past, check your medicine cabinet to make sure you don’t have any leftovers. Over half of all people with a history of opioid misuse report having gotten or stolen them from a friend or family member.
The best way to dispose of extra medications is through a program in your community. In the meantime, there are places throughout the greater Toledo area where you can deposit unwanted prescription medications safely and easily or check out what places are nearer to you in your county online.
Recognizing the Signs of Opioid Misuse:
According to the AMA, 45% of people who use heroin started with an addiction to prescription opioids. Because people usually receive their initial prescriptions from honest doctors trying to alleviate legitimate pain, some individuals labor under the misconception that these medications are safer than illegal drugs. The fact of the matter is that the potential for abuse and even addiction is very real, and addiction has been known to take hold after just one week of regular use.
For people who are concerned that their child, loved one or friend is misusing opioids, look for the signs. Mood swings or constant irritability may describe the majority of teenagers, but in their extreme form it could indicate a more serious problem. Losing a job or failing in school can also be a red flag, as can disappearing for long periods of time, stealing money or frequent flu-like symptoms. Of course, be on the lookout for more obvious signs such as puncture marks on the arms or excessively lethargic behavior.
Stage 3: Getting Help for People Fighting Opioid Addiction
The AMA also offers pointers on what to do when you’re dealing with someone contending with serious opioid misuse, including knowing the signs of an overdose. These may include:
- Slowed or no breathing
- Unconsciousness
- Confusion
- Nervousness
- Pinpoint pupils
- Clammy skin
- Fatigue
- Seizures
If someone you know is misusing opioids, it may be a good idea to keep Naloxone – Narcon (a narcotic antidote) on hand. Naloxone reverses the effects of opioids and can help preventing death from an overdose until healthcare professionals can arrive. Naloxone is available at a number of pharmacies throughout the U.S. without a prescription, and is recommend you confer with your doctor to see if Naloxone is right for your loved one.
QUOTE FOR FRIDAY:
“Most people are familiar with many of the benefits of exercise, such as improving muscle strength and endurance, reducing the risk for heart disease and stroke, and preventing obesity. Perhaps not as well understood is the importance of regular physical activity in building and maintaining healthy bones. Inactivity causes loss of bone!
Aging, along with certain diseases and medications, can cause bones to become very weak and fragile over time — a condition called osteoporosis. It often occurs in women after menopause, and in men in older age. This bone-thinning disease puts people at a greater risk for broken bones, which can seriously limit mobility and independence. We also tend to lose muscle as we age — a condition called sarcopenia. People who develop osteoporosis or sarcopenia are considered frail: more likely to fall and more likely to break a bone.”
OrthoInfo (https://orthoinfo.aaos.org/en/staying-healthy/exercise-and-bone-health/)
The key to Healthy BONES!
The infrastructure of the human body that allows us to perform our daily activities from standing, to sitting, to walking, or even climbing is our skeletal system. The major pillar or beam in the skeletal system is the vertebral column (spinal column). This bone structure allows us to bend, stand upright, twist, to dancing up a storm down the happy trail of life, if taken care of properly. If not, you may not be considering your life a happy tune, during that time of injury that can be a short or long haul before resolved, if ever. This infrastructure is so vital in our activities of our daily life. Many of us don’t realize that until the injury or damage sets in. There is one way you can bypass this disaster, don’t have it become a part of your life which is taking preventative measures; especially if you do heavy lifting in your life; like in my job as a nurse. One major ingredient to preventative measures is proper body mechanics but the trick here is never lift heavy items from below your waist level without bending your legs or even better without a second person helping you or some form of support but there is more to it than just that. There are more factors involved in helping you keep your back with all other bones strong. That would be healthy dieting, maintaining a good weight for your height (body mass index), and good exercise (not necessarily work out but if that is what you enjoy doing, it’s even better and don’t stop). All these ingredients to a better development and maintenance of your skeletal system=HEALTHY HABITS. A plus and benefit that many choose to do is going regularly to a chiropractor who can keep your spine in alignment (see one before injury starts). Recommended in Rockland County, NY is Dr. Diane Gregory, who I go to for my back and who has done both prevention & Rx; www.gregorychiropractic.com.
The key is to be living a healthy life. This consists of diet, exercise, activity and healthy habits learned and practiced in your routine of daily living that will help prevent or assist you in treating bone and back injuries; even problems caused by the inactivity with doing heavy lifting (Ex. lack of any muscle tone or muscle knots), which can inflict bone or back injuries. The better we treat ourselves EVERYDAY regarding health the higher the odds we will live a longer life. One common problem in America that can occur if not living healthy and/or using improper body mechanics with heavy lifting, especially frequently, can increase the risk of sciatica nerve damage. The pain of sciatica is typically felt from the low back (lumbar area) to behind the thigh and radiating down below the knee. The sciatica nerve is the largest nerve in the body that begins from nerve roots in the lumbar spinal cord in the low back and extends through the buttock to send the nerve ending down the lower limb to the foot. Depending on the precise cause of the sciatica symptoms with the duration, the outlook for recovery from sciatica ranges from excellent to having long term chronic symptoms. This can be prevented to some extent by avoiding low back trauma injuries. Thinking before lifting is the one of the best ideas. Osteoporosis is a common bone problem that is a abnormal loss of bony tissue resulting in fragile porous bones attributable to a lack of calcium, most common in postmenopausal women. This progressive bone disease that’s characterized by a decrease in bone mass and density leads to an increased risk of a fracture. The causes of this disease that are modifiable (can be changed) would be: Vitamin D deficiency, menopause, excess alcohol, tobacco smoking, malnutrition (identified risk factors include low dietary calcium and/or phosphorus, magnesium, zinc, boron, iron, fluoride, copper, vitamins A,K,E, and C; also D where skin exposure to sunlight provides an inadequate supply. Excess sodium is a risk factor. High blood acidity may be diet related, and is a known antagonist to the bone. Some have identified low protein intake as associated with lower peak bone mass during adolescence and lower bone mineral density in elderly populations. Other risk factors are inactive, underweight, heavy leads-a strong association between cadmium and lead with bone disease has been established. Low-level exposure to cadmium is associated with an increased loss of bone mineral density readily in both genders. Some studies even show soft drinks can increase the risk of osteoporosis related to high phosphoric acid. Others suggest soft drinks may displace calcium containing drinks from the diet rather than causing osteoporosis.
Another bone disorder is osteomalacia that is a softening of the bones caused by defective bone mineralization secondary to inadequate amounts of available phosphorus and calcium. The most common cause of the disease is a deficiency in vitamin D, which is normally obtained from the diet and/or from sunlight exposure. We can help our bones in many ways. There is not just one food to eat or one type of exercise to do or one healthy habit to practice to keep you healthy with strong bones, there are choices. Wouldn’t you want less risk of bone or back injury or disease for yourself and for others throughout the nation including the future generations? Than join me and others. If you like what you see spread the good cheer. Let’s build a stronger foundation regarding HEALTH in America.
Adults need 700mg of calcium a day. You should be able to get all the calcium you need by eating a varied and balanced diet.
Foods healthy for bones and Good sources of calcium include::
- milk, cheese and other dairy foods.
- green leafy vegetables, such as broccoli, cabbage and okra, but not spinach.
- soya beans.
- tofu.
- plant-based drinks (such as soya drink) with added calcium.
- nuts.
- bread and anything made with fortified flour.
- fish where you eat the bones, such as sardines and pilchards.
QUOTE FOR WEDNESDAY:
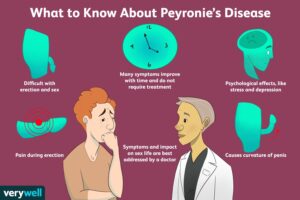
“Peyronie disease rarely goes away on its own. In most people with the condition, it will remain as is or may get slightly worse early on. Early treatment soon after you get the condition may keep it from getting worse or even improve symptoms. Even if you’ve had Peyronie disease for some time, treatment may help ease symptoms such as pain, curving and shortening.”
MAYO CLINIC (https://www.mayoclinic.org/diseases-conditions/peyronies-disease/symptoms-causes/syc-20353468)
Part II Peyronie’s Disease – how its diagnosed and treatments.
How the Diagnosis of Peyronie’s Disease is made:
Health care professionals often can figure out if someone has Peyronie disease by doing a physical exam. They also might do tests to check for other conditions that can cause similar symptoms.
You might need the following tests:
- Physical exam. Your health care professional feels your penis when it’s not erect to figure out the location and amount of scar tissue. The length of your penis also might be measured. If the condition becomes worse, this measurement helps determine whether the penis has gotten shorter.Your health care professional also might ask you to bring in photos of your erect penis taken at home. This can help determine the degree of curving, the location of scar tissue or other details that might guide treatment.
- Other tests. Your health care professional might order an ultrasound or other tests to check your penis when it’s erect. Before testing, you’ll likely receive a shot directly into the penis that helps it become erect.Ultrasound is the most commonly used test for penis conditions. It uses sound waves to make images of soft tissues inside the body. These tests can show the presence of scar tissue, blood flow to the penis and any other irregular signs.
Treatment of Peyronie’s Disease:
Treatment options for Peyronie disease depend on how long it’s been since you began having symptoms.
- Acute phase. As scar tissue forms, changes in the curve or length of the penis become worse. You also may have pain during erections. The acute phase may last for 5 to 18 months.
- Chronic phase. The scar tissue in the penis stops growing, and your symptoms become stable. You also have no penile pain or changes in the curve, length or other aspects of the penis. The chronic phase happens later in Peyronie disease.
Acute phase Peyronie disease treatment
For the acute phase of the condition, treatments include:
- Traction therapy. When used early in the process, a device that holds the penis in a cradle and applies tension can be helpful. This is called penile traction therapy. It prevents length loss and limits curving.
- Medicines. Some medicines taken by mouth or given in shots are options in this phase. Some medicines that have been used in the past clearly do not work. Others may or may not help. Your health care professional will likely talk with you in more detail.
Surgery is not recommended in the acute phase of Peyronie disease. It isn’t a treatment option until the condition stops becoming worse and any pain goes away. This lowers the chances of needing a second surgery.
Chronic phase Peyronie disease treatment
For the chronic phase of the disease, treatment choices include:
- Watchful waiting, in which your health care team watches your condition closely and gives treatment if your symptoms become worse.
- Injections or shots into the scar tissue.
- Stretching devices, also called “traction” therapy.
- Surgery to straighten the penis.
These treatments may be done alone or combined with one another.
Oral medications taken by mouth aren’t recommended in the chronic phase. They haven’t been shown to be effective at this stage of the disease.
QUOTE FOR TUESDAY:
“Peyronie’s (pay-roe-NEEZ) disease is a condition in which scar tissue (plaque) in your penis causes it to bend, curve or lose length or girth (circumference). You may be able to feel the scar tissue through your skin, or you may have pain in a specific part of your penis as the scar tissue forms.”
Cleveland Clinic (https://my.clevelandclinic.org/health/diseases/10044-peyronies-disease)
Part I Peyronie’s Disease
Erectile dysfunction (impotence) is the inability to get and keep an erection firm enough for sex.
Having erection trouble from time to time isn’t necessarily a cause for concern. If erectile dysfunction is an ongoing issue, however, it can cause stress, affect your self-confidence and contribute to relationship problems. Problems getting or keeping an erection can also be a sign of an underlying health condition that needs treatment and a risk factor for heart disease.
If you’re concerned about erectile dysfunction, talk to your doctor — even if you’re embarrassed. Sometimes, treating an underlying condition is enough to reverse erectile dysfunction. In other cases, medications or other direct treatments might be needed.
Symptoms
Erectile dysfunction symptoms might include persistent:
- Trouble getting an erection
- Trouble keeping an erection
- Reduced sexual desire
When to see a doctor
A family doctor is a good place to start when you have erectile problems. See your doctor if:
- You have concerns about your erections or you’re experiencing other sexual problems such as premature or delayed ejaculation
- You have diabetes, heart disease or another known health condition that might be linked to erectile dysfunction
- You have other symptoms along with erectile dysfunction
Causes
Male sexual arousal is a complex process that involves the brain, hormones, emotions, nerves, muscles and blood vessels. Erectile dysfunction can result from a problem with any of these. Likewise, stress and mental health concerns can cause or worsen erectile dysfunction.
Sometimes a combination of physical and psychological issues causes erectile dysfunction. For instance, a minor physical condition that slows your sexual response might cause anxiety about maintaining an erection. The resulting anxiety can lead to or worsen erectile dysfunction.
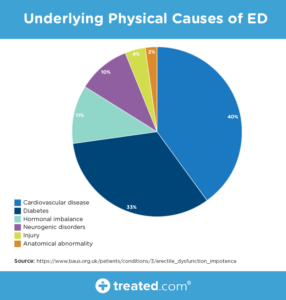
Physical causes of erectile dysfunction
In many cases, erectile dysfunction is caused by something physical. Common causes include:
- Heart disease
- Clogged blood vessels (atherosclerosis)
- High cholesterol
- High blood pressure
- Diabetes
- Obesity
- Metabolic syndrome — a condition involving increased blood pressure, high insulin levels, body fat around the waist and high cholesterol
- Parkinson’s disease
- Multiple sclerosis
- Certain prescription medications
- Tobacco use
- Peyronie’s disease — development of scar tissue inside the penis
- Alcoholism and other forms of substance abuse
- Sleep disorders
- Treatments for prostate cancer or enlarged prostate
- Surgeries or injuries that affect the pelvic area or spinal cord
Psychological causes of erectile dysfunction
The brain plays a key role in triggering the series of physical events that cause an erection, starting with feelings of sexual excitement. A number of things can interfere with sexual feelings and cause or worsen erectile dysfunction. These include:
- Depression, anxiety or other mental health conditions
- Stress
- Relationship problems due to stress, poor communication or other concerns
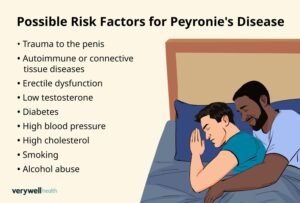
Risk factors
As you get older, erections might take longer to develop and might not be as firm. You might need more direct touch to your penis to get and keep an erection.
Various risk factors can contribute to erectile dysfunction, including:
- Medical conditions, particularly diabetes or heart conditions
- Tobacco use, which restricts blood flow to veins and arteries, can — over time — cause chronic health conditions that lead to erectile dysfunction
- Being overweight, especially if you’re obese
- Certain medical treatments, such as prostate surgery or radiation treatment for cancer
- Injuries, particularly if they damage the nerves or arteries that control erections
- Medications, including antidepressants, antihistamines and medications to treat high blood pressure, pain or prostate conditions
- Psychological conditions, such as stress, anxiety or depression
- Drug and alcohol use, especially if you’re a long-term drug user or heavy drinker
Complications
Complications resulting from erectile dysfunction can include:
- An unsatisfactory sex life
- Stress or anxiety
- Embarrassment or low self-esteem
- Relationship problems
- The inability to get your partner pregnant
Prevention
The best way to prevent erectile dysfunction is to make healthy lifestyle choices and to manage any existing health conditions. For example:
- Work with your doctor to manage diabetes, heart disease or other chronic health conditions.
- See your doctor for regular checkups and medical screening tests.
- Stop smoking, limit or avoid alcohol, and don’t use illegal drugs.
- Exercise regularly.
- Take steps to reduce stress.
- Get help for anxiety, depression or other mental health concerns.