Psoriasis August Awareness Month – When to see your doctor, Causes, Risk Factors & Complications!
When to see a doctor
If you suspect that you may have psoriasis, see your doctor for an examination. Also, talk to your doctor if your psoriasis:
- Causes you discomfort and pain
- Makes performing routine tasks difficult
- Causes you concern about the appearance of your skin
- Leads to joint problems, such as pain, swelling or inability to perform daily tasks
Seek medical advice if your signs and symptoms worsen or don’t improve with treatment. You may need a different medication or a combination of treatments to manage the psoriasis.
Causes
The cause of psoriasis isn’t fully understood, but it’s thought to be related to an immune system problem with T cells and other white blood cells, called neutrophils, in your body.
T cells normally travel through the body to defend against foreign substances, such as viruses or bacteria.
But if you have psoriasis, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
Overactive T cells also trigger increased production of healthy skin cells, more T cells and other white blood cells, especially neutrophils. These travel into the skin causing redness and sometimes pus in pustular lesions. Dilated blood vessels in psoriasis-affected areas create warmth and redness in the skin lesions.
The process becomes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Skin cells build up in thick, scaly patches on the skin’s surface, continuing until treatment stops the cycle.
Just what causes T cells to malfunction in people with psoriasis isn’t entirely clear. Researchers believe both genetics and environmental factors play a role.
Psoriasis triggers
Psoriasis typically starts or worsens because of a trigger that you may be able to identify and avoid. Factors that may trigger psoriasis include:
- Infections, such as strep throat or skin infections
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn
- Stress
- Smoking
- Heavy alcohol consumption
- Vitamin D deficiency
- Certain medications — including lithium, which is prescribed for bipolar disorder, high blood pressure medications such as beta blockers, antimalarial drugs, and iodides
Risk factors
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. This is one of the most significant risk factors. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Lesions (plaques) associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
Complications
If you have psoriasis, you’re at greater risk of developing certain diseases. These include:
- Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
- Eye conditions. Certain eye disorders — such as conjunctivitis, blepharitis and uveitis — are more common in people with psoriasis.
- Obesity. People with psoriasis, especially those with more severe disease, are more likely to be obese. It’s not clear how these diseases are linked, however. The inflammation linked to obesity may play a role in the development of psoriasis. Or it may be that people with psoriasis are more likely to gain weight, possibly because they’re less active because of their psoriasis.
- Type 2 diabetes. The risk of type 2 diabetes rises in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
- High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
- Cardiovascular disease. For people with psoriasis, the risk of cardiovascular disease is twice as high as it is for those without the disease. Psoriasis and some treatments also increase the risk of irregular heartbeat, stroke, high cholesterol and atherosclerosis.
- Metabolic syndrome. This cluster of conditions — including high blood pressure, elevated insulin levels and abnormal cholesterol levels — increases your risk of heart disease.
- Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn’s disease are more likely to strike people with psoriasis.
- Parkinson’s disease. This chronic neurological condition is more likely to occur in people with psoriasis.
- Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
- Emotional problems. Psoriasis can also affect your quality of life. Psoriasis is associated with low self-esteem and depression. You may also withdraw socially.
QUOTE FOR WEDNESDAY:
“National Immunization Awareness Month (NIAM) is an annual observance held in August to highlight the importance of vaccination for people of all ages”
Centers for Disease Control and Prevention
“Vaccines work by stimulating the body’s immune system to safely provide protection against viruses or bacteria that cause infection. After vaccination, the immune system is prepared to respond quickly when the body encounters the disease-causing organism.”.
Federal and Drug Administration FDA
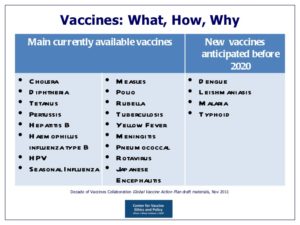
National Immunization Awareness Month
National Immunization Awareness Month (NIAM) is an annual observance held in August to highlight the importance of vaccination for people of all ages. NIAM was established to encourage people of all ages to make sure they are up to date on the vaccines recommended for them. Communities have continued to use the month each year to raise awareness about the important role vaccines play in preventing serious, sometimes deadly, diseases.
Types of Vaccines:
Even with advances in health care, the diseases that vaccines prevent can still be very serious – and vaccination is the best way to prevent them; Including COVID!
The Immune System
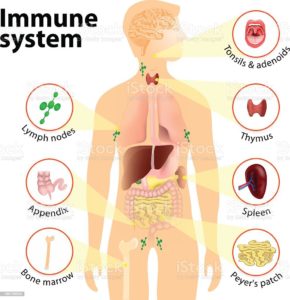
We hear those 2 words “Immune System “a lot; what is the immune system? The main parts of the immune system are:
- white blood cells.
- antibodies.
- complement system.
- lymphatic system.
- spleen.
- bone marrow.
- thymus.
Your immune system is a large network of organs, white blood cells, proteins (antibodies) and chemicals. This system works together to protect you from foreign invaders (bacteria, viruses, parasites, and fungi) that cause infection, illness and disease.
What does the immune system do and how does it work?
Your immune system works hard to keep you healthy. Its job is to keep germs out of your body, destroy them or limit the extent of their harm if they get in.
When your immune system is working properly: When your immune system is working properly, it can tell which cells are yours and which substances are foreign to your body. It activates, mobilizes, attacks and kills foreign invader germs that can cause you harm. Your immune system learns about germs after you’ve been exposed to them too. Your body develops antibodies to protect you from those specific germs. An example of this concept occurs when you get a vaccine. Your immune system builds up antibodies to foreign cells in the vaccine and will quickly remember these foreign cells and destroy them if you are exposed to them in the future. Sometimes doctors can prescribe antibiotics to help your immune system if you get sick. But antibiotics only kill certain bacteria. They don’t kill viruses.
When your immune system is not working properly: When your immune system can’t mount a winning attack against an invader, a problem, such as an infection, develops. Also, sometimes your immune system mounts an attack when there is no invader or doesn’t stop an attack after the invader has been killed. These activities result in such problems as autoimmune diseases and allergic reactions.
Your immune system is made of up a complex collection of cells and organs. They all work together to protect you from germs and help you get better when you’re sick. The main parts of the immune system are:
- White blood cells: Serving as an army against harmful bacteria and viruses, white blood cells search for, attack and destroy germs to keep you healthy. White blood cells are a key part of your immune system. There are many white blood cell types in your immune system. Each cell type either circulates in your bloodstream and throughout your body or resides in a particular tissue, waiting to be called into action. Each cell type has a specific mission in your body’s defense system. Each has a different way of recognizing a problem, communicating with other cells on the defense team and performing their function.
- Lymph nodes: These small glands filter and destroy germs so they can’t spread to other parts of your body and make you sick. They also are part of your body’s lymphatic system. Lymph nodes contain immune cells that analyze the foreign invaders brought into your body. They then activate, replicate and send the specific lymphocytes (white blood cells) to fight off that particular invader. You have hundreds of lymph nodes all over your body, including in your neck, armpits, and groin. Swollen, tender lymph nodes are a clue that your body is fighting an infection.
- Spleen: Your spleen stores white blood cells that defend your body from foreign invaders. It also filters your blood, destroying old and damaged red blood cells.
- Tonsils and adenoids: Because they are located in your throat and nasal passage, tonsils and adenoids can trap foreign invaders (for example, bacteria or viruses) as soon as they enter your body. They have immune cells that produce antibodies to protect you from foreign invaders that cause throat and lung infections.
- Thymus: This small organ in your upper chest beneath your breast bone helps mature a certain type of white blood cell. The specific task of this cell is to learn to recognize and remember an invader so that an attack can be quickly mounted the next time this invader is encountered.
- Bone marrow: Stem cells in the spongy center of your bones develop into red blood cells, plasma cells and a variety of white blood cells and other types of immune cells. Your bone marrow makes billions of new blood cells every day and releases them into your bloodstream.
- Skin, mucous membranes and other first-line defenses: Your skin is the first line of defense in preventing and destroying germs before they enter your body. Skin produces oils and secretes other protective immune system cells. Mucous membranes line the respiratory, digestive, urinary and reproductive tracts. These membranes secrete mucus, which lubricates and moistens surfaces. Germs stick to mucus in the respiratory tract and then are moved out of the airways by hair-like structures called cilia. Tiny hairs in your nose catch germs. Enzymes found in sweat, tears, saliva and mucus membranes as well as secretions in the vagina all defend and destroy germs.
- Stomach and bowel: Stomach acid kills many bacteria soon after they enter your body. You also have beneficial (good) bacteria in your intestines that kill harmful bacteria.
QUOTE FOR THE WEEKEND:
“Menopause is a point in time when you’ve gone 12 consecutive months without a menstrual cycle. The time leading up to menopause is called perimenopause. This is when a lot of women or people assigned female at birth (AFAB) start to transition to menopause. They may notice changes in their menstrual cycles or have symptoms like hot flashes. Natural menopause is the permanent ending of menstruation that doesn’t happen because of any type of medical treatment. The process is gradual and happens in 3 stages. The average age of menopause in the United States is approximately 51 years old. However, the transition to menopause usually begins in your mid-40s. “.
Cleveland Clinic (https://my.clevelandclinic.org/health/diseases/21841-menopause)
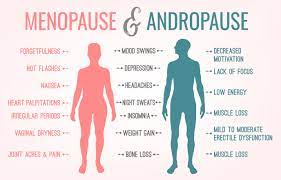
Menopause and it’s effects on women’s health.
What is Menopause exactly?
Menopause is when the ovaries naturally stop producing 2 hormones called estrogen and progesterone. Your ovaries are similar to what a car does in that over years it wears down, well so does the mechanism that regulates your hormones which is the ovaries. You go 12 consecutive months without having a period with no reasons to be explained for its occurrence, both biological or physical with it never returning. If both ovaries are removed surgically the menopause kicks in immediately. Menopause has signs and symptoms (s/s) that kick in which have varying intensities (it depends on the individual). You may experience mild to severe s/s.
Menopause is the time that marks the end of your menstrual cycles. It’s diagnosed after you’ve gone 12 months without a menstrual period. Menopause can happen in your 40s or 50s, but the average age is 51 in the United States. Menopause is a natural biological process.
The signs and symptoms of Menopause :
1- Hot Flashes 2-Irregular Periods 3- Breast Pains 4- Night Sweats 5- Mood Swings 6- Loss of Labido 7- Vaginal Dryness 8-Brittle Nails 9-Bloating 10-Irritability 11-Depression 12- Weight Gain 13-Sleep Problems 14- Osteoporosis-one of the worst symptoms of menopause. 15-Loss of breast fullness in some. 16- Thinning of the hair and dry skin.
Did you know over 60% of adult Americans are considered obese or overweight?
Weight gain happens when a person increases their body mass, whether it is a result of fat deposits, additional muscle tissue, or excess fluid. However, weight gain associated with menopause typically involves increased amounts of fat around the abdomen. One of the most accurate ways to see if you are obese is to measure your body mass index which is free online, check out the internet. I do every so often.
Go to Free BMI Calculator – AICR.org
www.aicr.org/bmi calculator.
On average, a women gains about 12 to 15 pounds between the ages of 45 and 55, this is usually when menopause typically occurs. This extra weight generally does not evenly distribute itself throughout a woman’s body. The weight tends to accumulate around the abdomen instead and women often notice the shape of their bodies slowly losing their hour-glass figure.
What can resolve this issue?
We can’t stop menopause but their are things we can do in dealing with it.
As years progress the metabolism slows down; setting the physiological stage for weight gain. As a woman’s hormones fluctuate prior to menopause and preparing for a permanently reduced hormonal level, it is likely to experience weight gain.
So things that can be done:
Eat well and nutritious foods.
Exercise but balance with rest.
Keep up with regular visits with your doctor for preventive health care and any medical concerns. Continue getting these appointments during and after menopause.
Preventive health care as you age may include recommended health screening tests, such as colonoscopy, mammography and triglyceride screening. Your doctor might recommend other tests and exams, too, including thyroid testing if suggested by your history, and breast and pelvic exams.
QUOTE FOR FRIDAY:
“The aorta carries blood from the heart to the body. Aortic aneurysms can occur anywhere in the aorta. They may be tube shaped or round.
Aortic aneurysms include:
- Abdominal aortic aneurysm. An abdominal aortic aneurysm occurs along the part of the aorta that passes through the belly area.
- Thoracic aortic aneurysm. A thoracic aortic aneurysm occurs along the part of the aorta that passes through the chest cavity.”
MAYO CLINIC (https://www.mayoclinic.org/diseases-conditions/aortic-aneurysm/symptoms-causes/syc-20369472)
Some people may have both types of aortic aneurysms.
Having an aortic aneurysm increases the risk of developing a tear in the inner layer of the wall of the aorta. This tear is called an aortic dissection.
Part II Aortic Aneurysms –What’s inside it, What are the risk factors in getting this & the most common causes!
What is inside an aortic aneurysm?
The inside walls of aneurysms are often lined with a blood clot that forms because there is stagnant blood. The wall of an aneurysm is layered, like a piece of plywood.
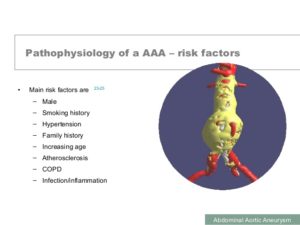
Who is most likely to have an abdominal aortic aneurysm?
Abdominal aortic aneurysms tend to occur in white males over the age of 60. In the United States, these aneurysms occur in up to 3.0% of the population. Aneurysms start to form at about age 50 and peak at age 80. Women are less likely to have aneurysms than men and African Americans are less likely to have aneurysms than Caucasians.
There is a genetic component that predisposes one to developing an aneurysm; the prevalence in someone who has a first-degree relative with the condition can be as high as 25%.
Collagen vascular diseases that can weaken the tissues of the aortic walls are also associated with aortic aneurysms. These diseases include Marfan and Ehlers-Danlos syndrome.
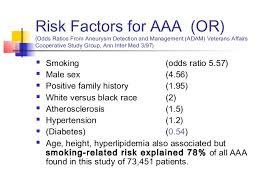
What are risk factors for aortic aneurysms?
The risk factors for aortic aneurysm are the same as those for atherosclerotic heart disease, stoke, and peripheral artery disease and include:
- Cigarette smoking: This not only increases the risk of developing an abdominal aortic aneurysm, but also increases the risk of aneurysm rupture. Aortic rupture is a life-threatening event where blood escapes the aorta and the patient can quickly bleed to death.
- High blood pressure
- Elevated blood cholesterol levels
- Diabetes mellitus The most common cause of aortic aneurysms is “hardening of the arteries” called arteriosclerosis. At a majority of aortic aneurysms are from arteriosclerosis. The arteriosclerosis can weaken the aortic wall and the increased pressure of the blood being pumped through the aorta causes weakness of the inner layer of the aortic wall.
- The aortic wall has three layers, the tunica adventitia, tunica media, and tunica intima. The layers add strength to the aorta as well as elasticity to tolerate changes in blood pressure. Chronically increased blood pressure causes the media layer to break down and leads to the continuous, slow dilation of the aorta.
- What is the most common cause of aortic aneurysms?
Smoking is a major cause of aortic aneurysm. Studies have shown that the rate of aortic aneurysm has fallen at the same rate as population smoking rates.
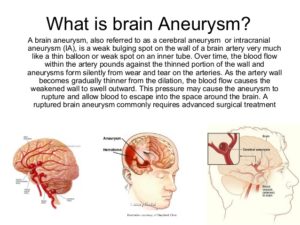
Know a aneurysm can be located in different arteries, like the brain with the same common causes, risk factors and make up inside the aneurysm.
QUOTE FOR THURSDAY:
“An aortic aneurysm is a balloon-like bulge in the aorta, the large artery that carries blood from the heart through the chest and torso. Facts about aortic aneurysms:
- Aortic aneurysms or aortic dissections were the cause of 9,904 deaths in 2019.1
- In 2019, about 59% of deaths due to aortic aneurysm or aortic dissection happen among men.1
- A history of smoking accounts for about 75% of all abdominal aortic aneurysms.2
- The U.S. Preventive Services Task Force recommends that men 65 to 75 years old who have ever smoked should get an ultrasound screening for abdominal aortic aneurysms, even if they have no symptoms.3“.
Centers for Disease Control and Prevention – CDC (https://www.cdc.gov/heartdisease/aortic_aneurysm.htm)