

Arthritis is inflammation of one or more of your joints. (Arthro=joint / itis = inflammation)
The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. Rheumatoid Arthritis symptoms are joint inflammation that comes from pain, warmth, and swelling. The inflammation is typically symmetrical that is occurring on both sides of the body at the same time (such as hands, wrists, or knees). Other signs of Rheumatoid Arthritis include joint stiffness that is particularly in the AM upon awakening or after periods of inactivity; ongoing fatigue, and low-grade fever. Signs and symptoms come about gradually over years but can come on rapidly for some other people.
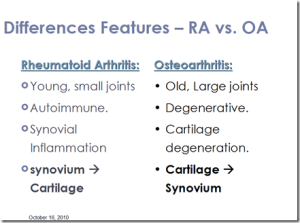
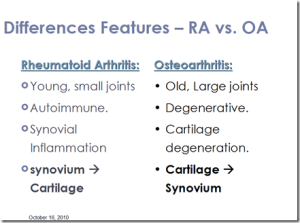
The two most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis is usually caused by normal wear and tear, while rheumatoid arthritis is an autoimmune disorder. Other types of arthritis can be caused by uric acid crystals, infections or even an underlying disease, such as psoriasis or lupus.
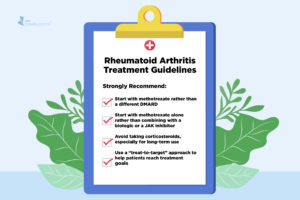
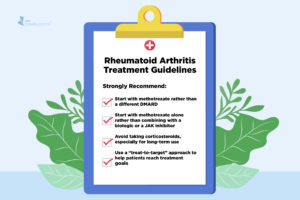
Treatments vary depending on the type of arthritis. The main goals of arthritis treatments are to reduce signs or symptoms and improve quality of life through Occupational or Physical Therapy and/or through medications, the old way.
Things that make arthritis worse: 1.) conventional medicine through doctors ordering medications (see Dr. David Brownstein’s website for his Natural Way to Health (with his book) to overcome arthritis). Drugs rarely CURE things. We are trained to believe doctors have all the answers with medications or surgeries in resolving our health problem. NOT THE CASE ALWAYS. It’s unnatural with arthritis and many other diagnoses. Natural therapies and good foods are not taken seriously by enough people in America in regards to helping a condition, like arthritis, or even prevention (which should be your first intervention, don’t wait for the diagnosis).
2.)Infection – check if a bacterial infection started your arthritis. If that is the cause antibiotics, low dose some doctors have given to people in studies and have worked. You would think this would be used more often, at least in testing for before just prescribing anti-inflammatory or analgesics meds. If its infection you need to kill the bacteria and the only way to do that it is with an antibiotic which kills a bacterial infection.
3.)DIET – Too many sugars or chemical preservatives and sweeteners which is in the standard American diet. Processed Foods are BAD. The same foods that cause obesity, diabetes and coronary artery disease can easily cause arthritis. Increase your fruits and nuts in your diet. Vitamin C and E are good for you. Pomegrante extract also.
4.) Dehydration- main causes of arthritis. Many simplify the problem. Your joints need water and if not enough it will cause an auto immune response=inflammation and get worse with processed foods.
5.) Heavy metal toxicity-Mercury, Arsenic and Nickel it includes. Not a fluke and mercury is one of the worst metals to have toxic in your body. Fish is the second worst source of heavy metal food. Few things you can do now, eat tuna occasionally. Silver malcum fillings have your dentist remove. Have your doctor do a heavy metal toxicity test on you if you never had one done and with arthritis.
6.) Low or imbalances of hormones=headache, faster aging, fatigue/lethargy, skin wrinkling sooner in life. Synthetic hormones don’t perform as well in your body and can lead to problems. Female hormones can increase your chance to breast cancer for example.
ACT America and one way to do that is go to Dr. David Brownstein website and check out Reverse your Arthritis to deal with your arthritis naturally and reading his books with bonuses.
Diet and bodyweight impact on arthritis
Experts say that eating a well-balanced diet is vital when you have arthritis. Not only will you be receiving critical nutrients, you will also be either maintaining or arriving more quickly at a healthy bodyweight. If you are overweight you will be adding extra pressure on weight-bearing joints. Many patients have found that losing just a few pounds made a significant difference to their quality of life. Doctors and nutritionists are more frequently advising arthritis patients to keep sugary and/or fatty foods to a minimum – such as red meat, cream and cheese. You should make sure you are eating plenty of fruit and vegetables, as well as whole grains. Omega-3 essential fatty acids are thought to relieve to some extent the symptoms of arthritis. A common source of Omega-3 fatty acids is oily fish, such as sardines, herring, trout, and salmon. The healthier our country the better our health care system will turn out for everyone.