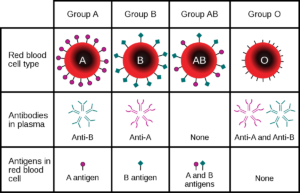
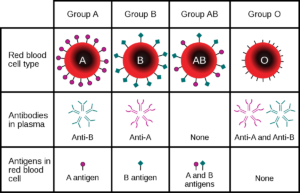
Blood type (also called blood group) is genetically determined. Blood is primarily categorised based on the presence and/or absence of antigens on the surface of our red blood cells (RBCs). Antigens are distinct molecules or substances capable of coaxing an immune response. Our immune system sends out mini soldiers called antibodies (also known as immunoglobulins), which are special proteins that recognise and bind to these antigens.
If our antibodies recognise these antigens as allies or naturally part of our body, our immune system happily leaves it alone. But if they detect enemy or foreign antigens, our immune system will go on an all-out war to destroy them. This is the reason you need give the blood type and Rh factor (positive or negative) that a patient is if they need blood transfusions to prevent this destructive action to take place unless your the universal donor type O with no antibodies. Unfortunately, our immune system isn’t perfect. In rare cases, it does attack ‘self’ antigens, as seen in some cases of autoimmune blood disorders.
You might be familiar with the ABO blood group system. When you ask someone what blood type they are, they might respond with “AB”. They are referring to this most important blood group system in human-blood transfusion. It comprises of only two antigens (antigen A and antigen B), but it can produce these four ABO blood types: A, B, AB or O. At present, the International Society of Blood Transfusion recognises 36 human blood group systems and more than 300 different antigens. The most common are type ABO and AB blood types.
Why does Rh positive or negative matter in knowing for your blood type?
The Rh blood group system has a colourful history. It consists of 61 blood group antigens (Rh antigens), which are expressed as part of a protein complex found only in RBC membranes. Rh antigens are believed to be essential for maintaining the integrity of RBCs.
Briefly going back to ABO blood group system, some people might tell you that they’re “O negative” or “A positive”. The negative/positive part refers to the absence or presence of one Rh antigen: the Rh(D) antigen. It’s the main Rh antigen considered for human-blood transfusion.
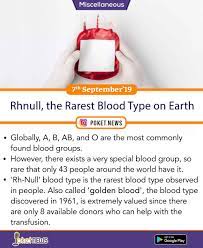
So what is Rh Null?
People who have the ‘golden blood’ type lack these Rh antigens. Their DNA lacks the genes responsible for building those RBC protein complexes. These people don’t just lack one, two or three of these 61 Rh antigens, they actually lack all of them. Yes, you read that right: all of them. As you might have guessed, people with Rh Null blood type have abnormal RBCs. They have deformed shapes, leaky membranes and shorter lifespans, which sometimes result in mild anaemia for the individual. Still, the absence of all Rh antigens makes Rh null the ‘golden blood’, which is highly admired for its rarity and medical purposes.
Rare blood types within the Rh blood type system can make it difficult or even impossible to get a blood transfusion. This makes Rh Null blood as the ‘universal’ life-saving blood for the Rh blood type system (especially if the donor has an ABO blood type O too).
But rarity comes at a price. If people with Rh Null blood type requires a blood transfusion, they can only receive Rhnull blood themselves. Even if they receive an O-negative blood, the presence of other Rh antigens on the RBCs may trigger a severe immune response. Therefore, these ‘golden blood’ carriers are solely dependent on other Rh Null donors, but only a few of them regularly donate and they are all spread out across the world.
This is why Rh Null blood is considered as the ‘golden blood’, but it’s not all sunshine and rainbows for those people who carry it. Still, we can’t deny the life-saving properties of this rare blood type and we can deeply appreciate the generosity of those selfless donors.