AMD/Low Vision Awareness Month
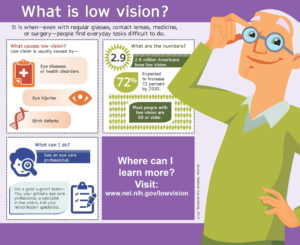
Prevent Blindness has declared February as Age-related Macular Degeneration (AMD) and Low Vision Awareness Month. According to the American Academy of Ophthalmology, AMD is a leading cause of vision loss in people 50 years or older, and more than 2.9 million Americans age 40 and older have low vision. Low vision is defined as a visual impairment that is not correctable through surgery, medicine, eye glasses or contact lenses.
According to the National Eye Institute, currently 4.2 million Americans ages 40 and older are visually impaired. Of these, 3 million have low vision. By 2030, when the last baby boomers turn 65, the number of Americans who have visual impairments is projected to reach 7.2 million, with 5 million having low vision.
For the millions of people who currently live or will live with low vision, the good news is that there is help.
But first, what is low vision? Low vision is when even with regular glasses, contact lenses, medicine, or surgery, people have difficulty seeing, which makes everyday tasks difficult to do. Activities that used to be simple like reading the mail, shopping, cooking, and writing can become challenging.
Most people with low vision are age 65 or older. The leading causes of vision loss in older adults are age-related macular degeneration, diabetic retinopathy, cataract, and glaucoma. Among younger people, vision loss is most often caused by inherited eye conditions, infectious and autoimmune eye diseases, or trauma. For people with low vision, maximizing their remaining sight is key to helping them continue to live safe, productive, and rewarding lives.
The first step is to seek help.
What is a low vision specialist? A low vision specialist is an ophthalmologist or optometrist who works with people who have low vision. A low vision specialist can develop a vision rehabilitation plan that identifies strategies and assistive devices appropriate for the person’s particular needs.
A low vision examination is quite different from the basic examination routinely performed by primary care optometrists and ophthalmologists.
A low vision examination includes a review of your visual and medical history, and places an emphasis on the vision needed to read, cook, work, study, travel, and perform and enjoy other common activities. The goals of a low vision exam include assessing the functional needs, capabilities, and limitations of your vision, assessing ocular and systemic diseases, and evaluating and prescribing low vision therapies.
Education and counseling of family and other care providers; providing an understanding of your visual functioning to aid educators, vocational counselors, employers and care givers; directing further evaluations and treatments by other vision rehabilitation professionals; and making appropriate referrals for medical intervention are all a part of a low vision evaluation.
Vision rehabilitation can include the following:
- Training to use magnifying and adaptive devices
- Teaching new daily living skills to remain safe and live independently
- Developing strategies to navigate around the home and in public
- Providing resources and support
The good news is that vision rehabilitation services can help people with vision impairment learn how to stay independent and make the most of their sight. Low Vision Awareness Month is a great time to spread the word about vision rehabilitation — and make sure that people with vision impairment know about the services available to them.
Magnification devices, electronic devices, computer-access software, and other access and mainstream technologies are used to help people with low vision maximize their remaining vision or learn alternative ways to do things, such as using their sense of touch or their sense of hearing.
QUOTE FOR FRIDAY:
“Sometimes, Waldenstrom macroglobulinemia (WM) isn’t causing any symptoms when it’s first found. Instead, it’s found when the person has blood tests done for some other reason. WM found this way is sometimes called asymptomatic or smoldering WM.
When WM does cause symptoms, some of them can be like those seen with other types of non-Hodgkin lymphoma (NHL). For example, weight loss, fever, night sweats, and swollen lymph nodes can be seen in many types of NHL.”
American Cancer Society/www.cancer.org (Signs and Symptoms of Waldenstrom Macroglobulinemia | American Cancer Society)
Part II Waldenstrom’s Macroglobulinemia (WM) & Lymphoplasmacytic Lymphoma (LPL)
Waldenstrom’s macroglobulinemia is named for the Swedish physician Jan Gosta Waldenström (1906-1996), who in 1944 identified a rare condition in which two patients experienced a thickening of their blood serum, bleeding of the mouth, nose, and blood vessels of the retina, low red blood cell and platelet counts, high erythrocyte sedimentation rates, and lymph node involvement. Bone marrow biopsies showed an excess of lymphoid cells and bone X-rays were normal, excluding a diagnosis of multiple myeloma. Both patients also had a large amount of a single unknown blood protein with an extremely high molecular weight, a “macro” globulin. We now know this globulin as IgM.
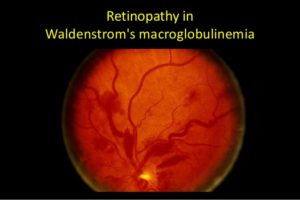
The over-production of IgM may also cause many of the symptoms associated with the disease. IgM is a large antibody and tends to make the blood thicker than normal, a condition called hyperviscosity. Unlike normal antibodies that fight infection, the IgM produced by WM cells has no useful function. Sometimes the IgM may incorrectly recognize the body’s tissues as “foreign” and attach to them, causing inflammation and injury.
What are the symptoms of this condition?
People with Waldenstrom’s macroglobulinemia may experience the following symptoms or signs. Sometimes, people with Waldenstrom’s macroglobulinemia do not have any of these changes. Or, the cause of a symptom may be a different medical condition that is not cancer.
- Fatigue
- Unexplained weight loss
- Enlarged lymph nodes or spleen
- Numbness, weakness or other nervous system problems, pain in the hands or feet, sometimes called peripheral neuropathy
- Abdominal swelling and diarrhea
- Weakness and shortness of breath
- Infections
- Raised pink or flesh-colored lesions on the skin
- Changes in the color of the fingertips when exposed to cold
- Changes in vision, which may include blurry vision or “double” vision
May signal a more aggressive cancer:
- Unexplained weight loss
- Unexplained fever
- Heavy sweating, especially at night, which may drench one’s nightclothes or sheets on the bed.
- Severe and/or extensive skin itchiness
How is it diagnosed?
For starters LAB TESTS:
WM might be suspected if your doctor finds you have low blood cell counts or unusual protein levels on blood tests. If so, your doctor may order a blood test called serum protein electrophoresis to find out what the abnormal proteins are. It is usually only after these tests are done that a biopsy of either the bone marrow or a lymph node is considered.
Simply a CBC Complete blood count, that measures the levels of red blood cells, white blood cells, and platelets. If lymphoma cells occupy too much of the bone marrow, these levels will be low.
Quantitative Immunoglobulins – This test measures the levels of the different antibodies (immunoglobulins) in the blood – IgA, IgE, IgG, and IgM – to see if any are abnormally high or low. In WM the level of IgM is high but the IgG level is often low.
Electrophoresis
The abnormal immunoglobulin made in WM is an IgM antibody. This antibody is monoclonal, meaning that it is many copies of the exact same antibody. Serum protein electrophoresi s (SPEP) is a test that measures the total amount of immunoglobulins in the blood and finds any monoclonal immunoglobulin. Another test, such as immunofixation or immunoelectrophoresis, is then used to determine the type of antibody that is abnormal (IgM or some other type).
Finding a monoclonal IgM antibody in the blood is needed to diagnose WM. This abnormal protein in WM is known by many different names, including monoclonal immunoglobulin M, IgM protein, IgM spike, IgM paraprotein, M protein, and M-spike. High levels of other types of monoclonal immunoglobulins, like IgA or IgG, are seen in different disorders (like multiple myeloma and some other lymphomas).
Sometimes pieces of the IgM protein are excreted by the kidneys into the urine. These proteins can be detected with a test called urine protein electrophoresis (or UPEP).
Viscosity
Viscosity is a measure of how thick the blood is. If the IgM level is too high, the blood will become thick (viscous) and can’t flow freely (think about pouring honey compared to pouring water).
Cryocrit
This test measures the blood levels of cryoglobulins (proteins that clump together in cool temperatures and can block blood vessels).
Cold agglutinins
Cold agglutinins are antibodies that attack and kill red blood cells, especially at cooler temperatures. These dead cells can then build up and block blood vessels. A blood test can be used to detect these antibodies.
Beta-2 microglobulin (β2M)
This test measures another protein made by the cancer cells in WM. This protein itself doesn’t cause any problems, but it’s a useful indicator of a patient’s prognosis (outlook). High levels of β2M are linked with a worse outlook.
Biopsies
The symptoms of WM and NHL are not distinctive enough for a doctor to know for certain if person has one of them, based on symptoms alone. Most symptoms can also be caused by non-cancerous problems like infections or by other kinds of cancers. Blood tests can help point to the correct diagnosis, but a biopsy (removing samples of affected tissue to look at under a microscope) is the only way to be sure. Several types of biopsies might be used.
Bone marrow aspiration and biopsy
This is the most important type of biopsy for WM, and is needed to confirm the diagnosis. It can be done at the doctor’s office or at the hospital.
The bone marrow aspiration and biopsy are usually done at the same time. The samples are taken from the back of the pelvic (hip) bone, although in some cases they may be taken from the sternum (breast bone) or other bones.
In bone marrow aspiration, you lie on a table (either on your side or on your belly). The doctor cleans the skin over the hip and then numbs the area and the surface of the bone by injecting a local anesthetic. This may briefly sting or burn. A thin, hollow needle is then inserted into the bone, and a syringe is used to suck out a small amount of liquid bone marrow. Even with the anesthetic, most patients still have some brief pain when the marrow is removed.
A bone marrow biopsy is usually done just after the aspiration. A small piece of bone and marrow is removed with a slightly larger needle that is pushed down into the bone. This may also cause some brief pain.
Once the biopsy is done, pressure is applied to the site to help stop any bleeding. There will be some soreness in the biopsy area when the numbing medicine wears off. Most patients can go home right after the procedure.
The bone marrow samples are then sent to a lab, where they are tested to see if they have lymphoma cells (see below). For a diagnosis of WM, at least 10% of the cells in the bone marrow must be lymphoplasmacytoid lymphoma cells.
Fine needle aspiration (FNA) biopsy
In an FNA biopsy, the doctor uses a very thin, hollow needle with a syringe to withdraw a small amount of tissue from a tumor or lymph node. This type of biopsy is useful for sampling lymph nodes to see if they are enlarged because of cancer or another cause such as infection. FNA can help diagnose some lymphomas, but WM is usually diagnosed with a bone marrow biopsy instead.
For an FNA on an enlarged node near the surface of the body, the doctor can aim the needle while feeling the node. If the enlarged node (or tumor) is deep inside the body, the needle can be guided while it is seen on a computed tomography (CT) scan or ultrasound (see the descriptions of imaging tests later in this section).
The main advantage of FNA is that it does not require surgery and can often be done in a doctor’s office. The main drawback is that in some cases it might not get enough tissue to make a definite diagnosis of lymphoma. However, advances in lab tests (discussed later in this section) and the growing experience of many doctors with FNA have improved the accuracy of this procedure.
Excisional or incisional biopsy
For these types of biopsies, a surgeon cuts through the skin to remove an entire lymph node or tumor (excisional biopsy) or a just a small part of a large tumor or lymph node (incisional biopsy). These biopsies are rarely needed in people with WM because the diagnosis is usually made with a bone marrow biopsy. They are used more often for other types of lymphoma.
If the area to be biopsied is near the skin surface, this can be done using local anesthesia (numbing medicine). If the area is inside the chest or abdomen, general anesthesia or deep sedation is used (where the patient is asleep). These types of biopsies almost always provide enough tissue to diagnose the exact type of lymphoma.
Fat pad fine needle aspiration
This type of biopsy may be used in some people with WM to check for amyloid. In this procedure, a thin, hollow needle with a syringe attached is inserted into an area of fat (usually under the skin of the abdomen/belly). A small amount of fat is removed and sent to the lab for testing.
Lab tests on biopsy specimens
All biopsy specimens are looked at under a microscope by a pathologist – a doctor with special training in using lab tests to diagnose diseases. In some cases, a hematopathologist, a doctor with further training in diagnosing blood and lymph node diseases, might also look at the biopsy. The doctors look at the size and shape of the cells and how the cells are arranged. Sometimes just looking at the cells doesn’t provide a clear answer, so other lab tests are needed.
Immunohistochemistry
In this test, a part of the biopsy sample is treated with special man-made antibodies that attach to cells only if they contain specific molecules. These antibodies cause color changes, which can be seen under a microscope. This test may help tell different types of lymphoma from one another and from other diseases.
Flow cytometry
In this test, cells are treated with special man-made antibodies. Each antibody sticks only to certain types of cells. The cells are then passed in front of a laser beam. If the cells now have antibodies attached to them, the laser will make them give off light, which is measured and analyzed by a computer.
This is the most common test for immunophenotyping – classifying lymphoma cells according to the substances (antigens) on their surfaces. Different types of lymphocytes have different antigens on their surface. These antigens also change as each cell matures.
This test can help show whether a lymph node is swollen because of lymphoma, some other cancer, or a non-cancerous disease. It has become very important in helping doctors determine the exact type of lymphoma so they can select the best treatment.
Cytogenetics
Doctors use this technique to look at the chromosomes (long strands of DNA) inside lymphoma cells. Cells (usually from the bone marrow) are first grown in the lab. Then the chromosomes are stained and looked at under a microscope. Because it takes time for the cells to start dividing, this test can take weeks.
In some lymphomas, the cells may have too many chromosomes, too few chromosomes, missing parts of chromosomes (called deletions), or other abnormalities. These changes can help identify the type of lymphoma. In WM, deletions are the most common type of chromosome change.
Molecular genetic tests
Molecular tests such as fluorescent in situ hybridization (FISH) and polymerase chain reaction (PCR) are not usually needed to diagnose WM, but they are sometimes used to diagnose other types of NHL. These tests look at the cells’ DNA without having to grow the cells in the lab first. The tests can give results in less time than cytogenetics and can be done on cells from different sources (like lymph nodes, blood, and bone marrow). They are generally used to look for specific chromosome or gene changes, not just any change.
Imaging tests
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive particles to produce pictures of the inside of the body. These tests are not needed to diagnose WM, but one or more of them might be done to help show the extent of the disease in the body.
Chest x-ray
An x-ray might be done to look at the chest for enlarged lymph nodes.
Computed tomography (CT) scan
The CT scan uses x-rays to make detailed cross-sectional images of your body. Unlike a regular x-ray, CT scans can show the detail in soft tissues (such as internal organs). This scan can help show if any lymph nodes or organs in your body are enlarged. CT scans are useful for looking for signs of lymphoma in the chest, abdomen, and pelvis.
Before the test, you may be asked to drink a contrast solution and/or get an intravenous (IV) injection of a contrast dye to better outline abnormal areas in the body. You might need an IV line through which the contrast dye is injected. The injection can cause some flushing (a feeling of warmth, especially in the face). Some people are allergic to the dye and get hives or a flushed feeling or, rarely, have more serious reactions like trouble breathing and low blood pressure. Be sure to tell the doctor if you have any allergies (especially iodine or shellfish) or have ever had a reaction to any contrast material used for x-rays. Medication can be given to help prevent and treat allergic reactions.
A CT scanner has been described as a large donut, with a narrow table that slides in and out of the middle opening. You need to lie still on the table while the scan is being done. CT scans take longer than regular x-rays, and some people might feel a bit confined by the ring while the pictures are being taken.
CT-guided needle biopsy: CT scans can also be used to guide a biopsy needle into a suspicious area. For this procedure, the patient lies on the CT scanning table while the doctor moves a biopsy needle through the skin and toward the area. CT scans are repeated until the needle is in the right place. A biopsy sample is then removed and sent to the lab to be looked at under a microscope.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans make detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. This test is rarely used in WM, but if your doctor is concerned about the brain or spinal cord, MRI is very useful for looking at these areas.
Sometimes a contrast material is injected into a vein to make some structures clearer. This contrast is not the same as the contrast used for CT scans, but allergic reactions can still occur. Again, medicine can be given to prevent and treat allergic reactions.
MRI scans take longer than CT scans – often up to an hour. You may have to lie inside a narrow tube, which is confining and can upset some people. Newer, more open MRI machines might be another option. The machine makes loud buzzing and clicking noises that some people find disturbing. Some places provide headphones or earplugs to help block this noise out.
Ultrasound
Ultrasound uses sound waves and their echoes to make pictures of internal organs or masses.
Ultrasound can be used to look at lymph nodes near the surface of the body or to look inside your abdomen for enlarged lymph nodes or organs such as the liver, spleen, and kidneys. (It can’t be used to look at organs or lymph nodes in the chest because the ribs block the sound waves.) It is sometimes used to help guide a biopsy needle into an enlarged lymph node.
For this test, a small, microphone-like instrument called a transducer is placed on the skin (which is first lubricated with a gel). It gives off sound waves and picks up the echoes as they bounce off the organs. A computer then converts the echoes into a black and white image on a screen.
This is an easy test to have, and it uses no radiation. For most ultrasounds, you simply lie on a table, and a technician moves the transducer over the part of your body being looked at.
Positron emission tomography (PET) scan
For a PET scan, a radioactive sugar (known as FDG) is injected into the blood. (The amount of radioactivity used is very low and will pass out of the body in a day or so.) Because cancer cells in the body grow quickly, they absorb large amounts of the sugar. You then lie on a table in the PET scanner for about 30 minutes while a special camera creates a picture of areas of radioactivity. The picture is not detailed like a CT or MRI scan, but it can provide helpful informa- tion about your whole body.
PET scans can help tell if an enlarged lymph node contains lymphoma or not. It can also help spot small areas that might be lymphoma, even if the area looks normal on a CT scan. These tests can be used to tell if a lymphoma is responding to treatment. They can also be used after treatment to help decide whether an enlarged lymph node still contains lymphoma or is merely scar tissue.
Many medical centers now use a machine that combines the PET scan with a CT scan (PET/CT scan). This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed appearance of that area on the CT scan.
Questions you might be thinking and would like answered.
Should I get a second opinion? If so when?
What treatments are approved for WM?
QUOTE FOR THURSDAY:
“Waldenstrom macroglobulinemia is a rare slow-growing cancer that affects your blood cells. It’s a type of non-Hodgkin’s lymphoma. (Healthcare providers may refer to this condition by the initials WM or the name lymphoplasmacytic lymphoma). WM happens when genetic mutations change certain blood cells, setting up a chain reaction of medical conditions that may be life-threatening. Providers can’t cure this condition, but they do have treatments that ease and sometimes eliminate its symptoms.”
ClevelandClinic.org (Waldenstrom Macroglobulinemia (Lymphoplasmacytic Lymphoma)
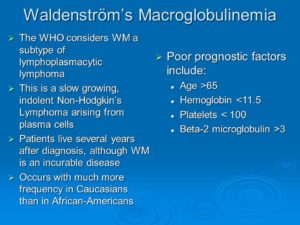
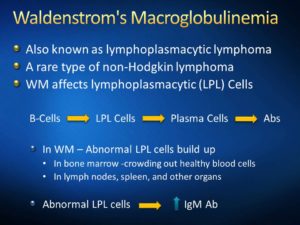
Part I Waldenstrom’s Macroglobulinemia (WM) also referred as Lymphoplasmacyctic Lymphoma (LPL)
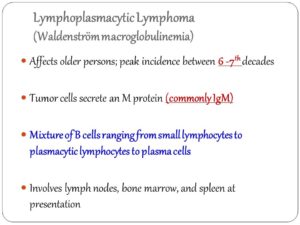
Affects older persons; peak incidence between 6 -7th decades. Tumor cells secrete an M protein (commonly IgM) Mixture of B cells ranging from small lymphocytes to plasmacytic lymphocytes to plasma cells. Involves lymph nodes, bone marrow, and spleen at presentation.
Initially, you will need to learn some basics about Waldenstrom’s macroglobulinemia (WM), sometimes referred to as a lymphoplasmacytic lymphoma (LPL). Newly diagnosed? Well striveforgoodhealth.com understands that this is a very difficult time for you. Not only are you, your family and your friends experiencing the gamut of different emotions that come with a cancer diagnosis, but there is so much new information to learn.
Here’s one place to start in getting information on this diagnosis!
Let’s understand first what is effected in the body and answer the questions that probably you are asking yourself (pt or family or friends).
What is effected in this disease?
B Lymphocytes are effected; they are a type of white blood cell that makes antibodies. B lymphocytes are part of the immune system and develop from stem cells in the bone marrow. Same with T cells. T- and B-cells are highly specialized defender cells – different groups of cells are tailored to different germs. When your body is infected with a particular germ, only the T- and B-cells that recognise it will respond. These selected cells then quickly multiply, creating an army of identical cells to fight the infection. Special types of T- and B-cells ‘remember’ the invader, making you immune to a second attack.
What’s so special about the B cells?
With the help of T-cells, B-cells make special Y-shaped proteins called antibodies. Antibodies stick to antigens on the surface of germs, stopping them in their tracks, creating clumps that alert your body to the presence of intruders. Your body then starts to make toxic substances to fight them. Patrolling defender cells called phagocytes engulf and destroy antibody-covered intruders.
With this disease what happens to the B Cells?
When diagnosed with Waldenstrom’s macroglobulinemia (WM) which is a lymphoma or cancer. It affects a type of white blood cell called a B-lymphocyte or B-cell, which normally matures into a plasma cell whose job is to manufacture immunoglobulins (antibodies) to help the body fight infection. In WM, there is a malignant change to the B-cell in the late stages of maturing and it continues to proliferate as a clone of identical cells, primarily in the bone marrow, but also in the lymph nodes and other tissues and organs. It is known as lymphoplasmacytic lymphoma (LPL) and must be associated with the production of an antibody protein or immunoglobulin known as IgM in order for WM to be diagnosed.
What’s the difference of WM versus LPL? Are they the same disease?
Sometimes WM and LPL (lymphoplasmacytic lymphoma) are used interchangeably although WM is really an LPL. However, WM comprises about 90 – 95% of all LPL patients.
The median survival has varied in studies, from 5 years to 10
QUOTE FOR WEDNESDAY:
“Dietary and lifestyle changes are the first step in treating GERD. Certain foods make the reflux worse. Suggestions to help alleviate symptoms include:
- Lose weight if you are overweight — of all of the lifestyle changes you can make, this one is the most effective.
- Avoid foods that increase the level of acid in your stomach, including caffeinated beverages.
- Avoid foods that decrease the pressure in the lower esophagus, such as fatty foods, alcohol and peppermint.”
John Hopkins Medicine (Gastroesophageal Reflux Disease (GERD) Treatment | Johns Hopkins Medicine)
Part II How to stay healthy with acid reflux-GERD.
Understanding what GERD is, its causes, its symptoms, the effects it has on your body and the way your body responds to specific treatments is necessary to help you devise a plan with your activities of daily living, including diet, to help manage the condition. If you haven’t seen my Part 1 just click on it onto my webpage than read yesterday’s article part 1 than read this. All you can do is apply your own GERD diet experimentation to the suggestions of others and try available treatments until you find what works for you. Also, there are foods that hve a reputation for being ‘safe’ (foods to avoid acid reflux) in most cases, as well as others that are known for being main contributors to acid reflux.
I recommend you go tohttp://www.gerd-diet.com which helps explain about foods and how they work with GERD. They do state the following:
Armoring Yourself with Patience and Willingness to Experiment (meaning this takes time in finding out what exacerbates your GERD and what helps it heal—Like an open wound, it takes time.) Sorry,There Is No One-Size-To-Fit-All With-A-GERD Diet (for relief or resolution)
Your Own Trigger Foods.
Given the complex nature of GERD, this one has to be added. I know it is repetitive, but everyone has certain foods that irritate their condition and causes severe symptoms. Make a list of these foods and avoid them in the future. This means make a journal for the next 2 weeks or more and see what caused your GERD symptoms to remember them with not eating fast which can cause GERD also (habit change).
GERD Diet FoodsA List of Food Groups and What Is Safe and Best to Avoid The following lists are comprised of foods that are typically known to be ‘safe’ or to ‘trigger’ symptoms.
Again, just because something is on the “avoid” list does not mean that you cannot eat it. Similarly, something appearing on the “safe” list does not guarantee that it will not cause a problem for you. This is simply provided as a guideline to give you a place to start and to make it easier for you design your own personal GERD diet.
|
FOOD GROUPS |
SAFE |
AVOID |
| FRUITS | Apples (fresh and dried), apple juice, bananas, pears, peaches, melons, strawberries, grapes | Oranges and orange juice, lemons and lemonade, grapefruit and grapefruit juice, tomato and tomato juice, cranberries and cranberry juice |
| VEGETABLES | Baked potato, broccoli, cabbage, carrots, green beans, peas, asparagus, lettuce, sweet potatoes | Raw onions, peppers, radishes, french fries, mashed potatoes |
| MEAT | Extra lean ground beef, steak (London Broil), skinless chicken breast, egg whites or substitute, fish (with no added fat), white turkey meat | Fatty ground beef, marbled sirloin, chicken nuggets, buffalo wings, fried meat |
| DAIRY | Feta or goat cheese, fat free cream cheese, fat free sour cream, low fat soy cheese | Whole milk, chocolate milk, ice cream, high fat cream cheese or sour cream |
| GRAINS | Cereal (bran or oatmeal), corn bread, graham crackers, pretzels, rice (brown or white), rice cakes, millet, quinoa | High fat grain products (cheese bread or products made with whole milk) |
| BEVERAGES | Water, herbal teas, non-citrus drinks, skimmed milk | Caffeinated beverages, whole milk, alcohol, carbonated beverages |
| FATS/OILS/CONDIMENTS | Low fat salad dressing, herbs ( basil, thyme, sage, oregano), hummus, mild sauces | Mustard, chili sauces, creamy salad dressing, black pepper, vinegar, curries, pickles, mint |
At this point, there is no alternative medicine therapies that have been accepted as proof for treatment(s) or 100% resolution for GERD.
However, like every other aspect of the disease, it really is an individual decision. Some people have reported natural remedies that have given amazing results with their GERD diet (healthier approach) while others find that prescription medications have little effect (meds can cause side effects temporary or permanently, depending on what it is).
GERD can be due obesity, lifestyle (unhealthy habits) and diet.
**It is recommended to see an MD first before making any decision on your own in treatment with a combination of or just one of the following: meds, diet or even health habit changes, especially for those people with disease/illness (s) present (Ex. Diabetes, cardiac disease, etc…).**
QUOTE FOR TUESDAY:
“Gastroesophageal reflux disease, or GERD, happens when acid from your stomach backs up into your esophagus, the tube connecting your stomach to your mouth.
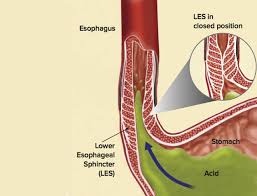
This digestive disorder affects the ring of muscle between your esophagus and your stomach. This ring is called the lower esophageal sphincter (LES). If you have GERD, you may get heartburn or acid indigestion. Doctors think that some people may have it because of a condition called hiatal hernia. In most cases, you can ease your GERD symptoms through diet and lifestyle changes. But some people may need medication or surgery.”
Web M.D. (WebMD.com/GERD: Symptoms, Causes, Treatments, Remedies for Relief)
What is GERD or ACID REFLUX? Learn the symptoms, complications, risk factors, & treatments.
What is acid reflux?
A gastrointestinal (GI) disease that is caused by a valve located between the esophagus and stomach, which normally is a strong muscular ring of tissue. This valve normally opens and closes completely preventing food backing up (called reflux) in the esophagus allowing the contents to reach the throat to the mouth. With acid reflux, what happens is this valve gets over expanded frequently to the point the valve gets overstretched and no longer fits over the opening between the esophagus and the stomach with a tight fit. Due to loss of the elasticity it now is allowing leakage from the stomach with both food and fluids going up the esophagus to the throat to the mouth due to the action of reflux, during the digestion process. What happens during digestion the stomach contents with digestive fluids from the stomach (which are acidic) are refluxed, that are NOT normally in the esophagus. In conclusion, reflux sends stomach contents that’s returning (an acidic environment) upward in the esophagus which is now in an environment not use to being exposed to the digestive fluids=acidity, which are needed to perform the digestion process of our foods/fluids that are in the stomach only. This leakage of the valve is the cause of this problem occurring=GERD or GASTROINTESTINAL REFLUX.
When you don’t have GERD food and fluids, the nutrients we swallow goes down the esophagus to the valve where it opens letting the contents into the stomach. Than digestion takes place in about 1-2 hours after eating with no feeling of heartburn or foods or fluids we ate don’t come back up in our throat to the mouth. Normally the valve is tight enough in preventing reflux=no leakage going back up to the mouth with food and acid during digestion (the primary purpose of its function). This means during digestion the food gets into the stomach which is broken down into smaller particles by the digestive acid fluids allowing the nutrients to pass into the bloodstream with the waste products staying in the stomach to reach the rectum. So when stomach digestion is complete it passes all the waste products onto the smaller intestines to the larger intestines to the rectum to be evacuated, without leakage or reflux. With GERD this contents does go backward sending it to the mouth again.
The signs and symptoms (s/s) of GERD or acid reflux:
1-Heartburn is the classic GERD symptom. It’s best described as a burning sensation in the chest and/or discomfort in the upper belly or abdomen accompanied by a feeling of fullness.
2- Regurgitation is the involuntary return of partially digested food from the stomach into the mouth. This uncomfortable symptom is commonly caused by GERD, since the esophageal sphincter (valve) is damaged to such a severe degree that the stomach juices (acidotic) can freely reflux to the level of the throat or mouth.
3-Pain present behind the sternum (chest pain) to the upper mid abdomen (where the stomach is). If severe call your M.D. or doctor to have evaluated (especially if in the chest).
4-Chronic cough to hoarseness 5-Recurrent pneumonias 6-Bloating 7-Nausea 8-Vomiting (yellow/green)
9-Lump in the throat 10-Difficulty swallowing 11-Chronic sore throat 12-Laryngitis 13-Post nasal drip
14-Ear Aches 15-Tooth decay or gingivitis (inflammation of the gums) or bad breath this is due to the acid fluids with the foods and fluids regurgitated back to the mouth from the stomach.
Complications that are caused by GERD when left untreated:
1-Narrowing of the esophagus called esophageal stricture. This is due to damage to cells in the lower esophageal from acid exposure that leads to scarring of the tissue. The scar tissue narrows the food pathway causing difficulty to swallow called dysphagia.
2-Esophagitis – inflammation of the esophagus. This constant backwash of acid can irritate the lining of your esophagus. Over time, the inflammation can cause complications such as bleeding or breathing problems leading into the next problem. 3-Esophageal Ulcers – Due to frequent exposure to acidic fluids and foods to the esophagus the mucosa gets irritated so bad it will even erode the mucosa causing skin ulceration. The esophagus environment is not use to the stomach’s = acidic. Take the outer skin of the body, if exposed long enough to acidic chemicals the skin will burn. Same principle for the esophagus constantly exposed to the environment of the stomach’s content of acidic fluids every time digestion takes place.
4-Precancerous changes to the esophagus (Barrett’s esophagus). In Barrett’s esophagus, the color and composition of the tissue lining the lower esophagus change. These changes are associated with risk of esophageal cancer. The risk of cancer is low. Cancer is rare but can happen (adenocarcinoma of the esophagus).
Risk factors:
Conditions that increase the risk of GERD would
include: Obesity, Pregnancy, Smoking, Dry Mouth, Diabetes, Asthma, Connective Tissue Disorders like scleroderma, delayed stomach empting, Zollinger-Ellison syndrome (ZES) (This is a rare disorder characterized by one or more tumors in the pancreas, duodenum, or both. The tumors cause the stomach to make too much acid, leading to peptic ulcers in the duodenum. The tumors are sometimes cancerous and spread to other areas of the body.).
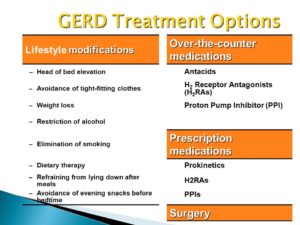
Treatment:
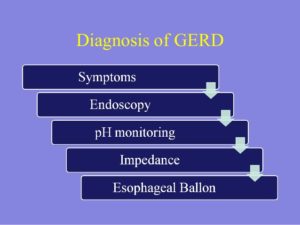
The key to treatment is prevention but if already diagnosed GERD than it would be maintenance. There is no one answer but start with being checked by your physician if you have any symptoms indicative of this diagnosis. Start with a getting a very good diagnostic tool ordered by your doctor called an Upper GI series (endoscopy) and when it’s done it will tell the M.D. a lot in what’s going on.
Then there is medications as a remedy, that can be useful, they are classified as proton pump inhibitors to H2 Inhibitors with more.
Another great key to the treatment is your LIFESTYLE=Diet (not eating acid foods, not eating fast), activity/exercise, your height compared to your weight (BMI or simply what you weigh) and lastly if you practice healthy vs. unhealthy habits.
If you would like to learn more about this come back tomorrow to my web page when I go further on the topic GERD (part 2) regarding the diet for the disease.