What Is the Worst Drug? introduces viewers to the dangers of fentanyl and the staggering mortality rates of nicotine and alcohol use.
For starters, that is a very complicated question because like, it depends on what kind of worst are you thinking about. And alcohol and nicotine are the most pervasive used drugs and because of that they also are accountable for a lot of deaths and also health issues because of prolonged use of these drugs or binge-like use of alcohol. And right now, in the US we have a very dangerous drug that is fentanyl that is a synthetic opioid that has been mixed into other drugs and is contaminating meth, coke, heroin and fentanyl is very potent and it can cause death.
1. Fentanyl is 50x more potent than heroin and when misused the consequences can be fatal. Know this is commonly used in OR where there is cardiac rhythm monitors and a RN watching the pt closely with maybe 3 more patients; possible less. That is how dangerous the drug is! Fentanyl earns the top spot on this list due to it being the most addictive, most powerful, and most deadly. This fully synthetic opioid is approximately 100 times more potent than morphine and is currently the number one cause of overdose fatality in the United States. Because of its strength, even a minuscule amount of fentanyl can cause a fatal overdose in an individual who has built up opioid tolerance. One kilogram of fentanyl has the potential to kill 500,000 people.
Drugs like methamphetamine and fentanyl are extremely dangerous for an individual who’s using them, but other substances are more dangerous for the population at large because so many people use these substances, and they can have dangerous effects. So, one example of that is nicotine. Smoking causes nearly 500, 000 related deaths a year which is a pretty staggering mortality rate. Alcohol is also used by many people and it can result in health problems, it can result in overdose death, it can also cause people to be in hazardous situations, to get into car accidents as a result of impaired driving. So, at a population level, since it’s much more used it is one of the worst substances.
2. Heroin is a central nervous system depressant and semi-synthetic opiate made from the drug morphine. When used, heroin suppresses breathing and reduces heart rate to dangerously low levels. As a depressant, this opioid is the source of many fatal overdoses and has largely contributed to the ongoing opioid epidemic.
As one of the most dangerous drugs on the planet, heroin may cause breathing cessation, heart infection, liver disease, collapsed veins, and death.The National Institute on Drug Abuse reports drug overdose deaths involving heroin rose from 1,960 in 1999 to 15,469 in 2016.
Any medication you take illegal and for a high especially through your vein is addictive!
3. Cocaineis a highly addictive stimulant that comes in powder form. When abused, the drug negatively impacts central nervous system functions and can cause stroke, cardiac arrhythmia, cardiac arrest, convulsions, and death. In 2017, drug overdose deaths involving cocaine increased by more than 34%, with almost 14,000 Americans dying from an overdose involving cocaine.
B. Crack cocaine is a form of powdered cocaine that has been chemically manipulated and hardened into a crystalline rock. Being a cheaper alternative to cocaine, crack is widely abused and extremely addictive. In 2016, there were an estimated 432,000 current crack users in the United States alone. The substance acts as a stimulant and causes irreversible bodily damage when abused.
Regardless of how much of the drug is used or how frequently, crack cocaine raises the danger of a heart attack, stroke, seizure, or respiratory failure, all of which can result in sudden death. In addition to the standard risks associated with cocaine use, crack users may experience serious respiratory troubles, including coughing, shortness of breath, lung damage, and bleeding. The heart, liver, and kidneys of long-term users of crack cocaine are severely harmed and users are more likely to be afflicted with infectious illnesses.
4. Methamphetamine is typically referred to as “meth”, this stimulant ranks within the top five most addictive, illicit drugs in the world. When used, meth produces a rush of euphoria, increased alertness, increased energy, and feelings of invincibility. Long-term meth use can lead to high blood pressure, heart attack, and stroke, in addition to harming your liver and kidneys. Meth can also cause your brain to permanently lose dopamine, which impairs memory, speech, and other mental functions.
Psychotic problems such as mood swings, paranoia, delusions, hallucinations, and violent and aggressive behavior are also likely to arise with prolonged meth use. Even after you have stopped using meth, you may continue to experience memory loss, confusion, and insomnia for months or years. According to the United States Drug Enforcement Administration, methamphetamine was the second-largest contributor to overdose deaths in the United States between May 2019 and May 2020.
5. Oxycodone is an extremely potent opioid prescription drug. It is often available in combination with other analgesics such as aspirin or acetaminophen. Due to it being twice as potent as morphine, oxycodone is highly addictive and life-threatening when abused. As stated in the CDC’s National Vital Statistics Report, oxycodone use ranked first in overdose deaths in 2011 with 5,587 overdose fatalities that year. It is legal by prescription only.
Oxycodone is commonly used in the hospital for pain.
6. Benzodiazepines They are a class of prescription drugs used to treat various anxiety and sleep disorders. According to data collected by the National Institute on Drug Abuse, the number of adults filling a benzodiazepine prescription increased 67%, from 8.1 million to 13.5 million between 1996 and 2013. Due to the sedative quality of benzos, they are at high risk for abuse and addiction. Although overdose fatalities from benzodiazepines are not common, the prescription drug is very dangerous when combined with other addictive substances such as alcohol or opioids.
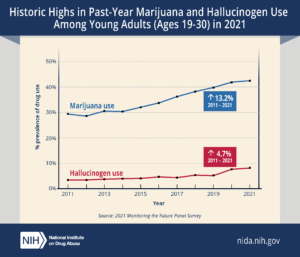
The Rise of Drug Use for Adults Ages 26-49
While young adults ages 18-25 have the highest rates of drug use across the board, drug use among adults ages 26-49 is on the rise:
- The percentage of adults age 26 and older using marijuana daily or almost daily has nearly doubled since 2015.
- Cocaine use and death rates have risen; cocaine-involved overdose rates in the U.S. have risen annually since 2012.
- Meth use is on the rise and overdose death rates climbed more than five-fold for those ages 25 to 54 between 2011 and 2018.
- The nation remains in a prescription and illicit opioids crisis, as 81,230 drug overdose deaths occurred in the U.S.—the highest single year ever reported—in the 12 months ending in May 2020; most of the overdose deaths involved a prescription or illicit opioid.