Multiple sclerosis (MS) is an unpredictable, often disabling disease of the central nervous system that disrupts the flow of information within the brain, and between the brain and body.
It can be a challenge for doctors to diagnose multiple sclerosis (MS). There’s no one test that can definitely show if someone has it. And there are many conditions with symptoms that can seem like MS.
But a neurologist who specializes in treating the disease should be able to look into how you’re feeling and help you figure out if your symptoms mean you have MS or another problem.
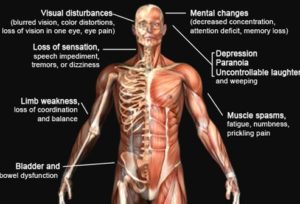
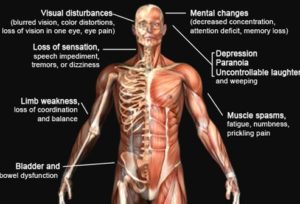
SYMPTOMS OF MULTIPLE SCLEROSIS:
Multiple Sclerosis symptoms vary from person to person but there are common symptoms with MS. Those could be the following:
*Fatigue-Occurs in about 80% of people, can significantly interfere with ability to function at home and work, and may be the most prominent symptom in a person who otherwise has minimal activity limitations.
*Difficulties with your walking gait-Related to several factors including weakness, spasticity, loss of balance, sensory deficit and fatigue, and can be helped by physical therapy, assistive therapy and medications.
*Numbness or Tingling-Numbness of the face, body, or extremities (arms and legs) is often the first symptom experienced by those eventually diagnosed as having MS.
*Spasticity-Refers to feelings of stiffness and a wide range of involuntary muscle spasms; can occur in any limb, but it is much more common in the legs.
*Weakness-Weakness in MS, which results from deconditioning of unused muscles or damage to nerves that stimulate muscles, can be managed with rehabilitation strategies.
*Visual Problems-The first symptom of MS for many people. Onset of blurred vision, poor contrast or color vision, and pain on eye movement can be frightening — and should be evaluated promptly.
*Dizziness or Vertigo-People with MS may feel off balance or lightheaded, and for some even much less often have the sensation that they or their surroundings are spinning (vertigo).
*Bladder Problems-Bladder dysfunction, which occurs in at least 80% of people with MS, usually can be managed quite successfully through dietary and fluid management, medications, and catheterization.
*Sexual Problems-Very common in the general population including people with MS. Sexual responses can be affected by damage in the central nervous system, as well by symptoms such as fatigue and spasticity, and by psychological factors.
*Bowel Function-Constipation is a particular concern among people with MS, as is loss of control of the bowels. Bowel issues can typically be managed through diet, adequate fluid intake, physical activity and medication.
*Pain-Pain syndromes are common in MS. In one study, 55% of people with MS had “clinically significant pain” at some time, and almost half had chronic pain.
*Cognitive changes-Refers to a range of high-level brain functions affected in 50% of people with MS, including the ability to learn and remember information, organize and problem-solve, focus attention and accurately perceive the environment.
*Emotional changes-Can be a reaction to the stresses of living with MS as well as the result of neurologic and immune changes. Bouts of depression, mood swings, irritability, and episodes of uncontrollable laughing and crying pose significant challenges for people with MS and their families.
*Depression-Studies have suggested that clinical depression — the severest form of depression — is among the most common symptoms of MS. It is more common among people with MS than it is in the general population or in persons with many other chronic, disabling conditions
Less common symptoms:
*Speech problems-this including slurring (dysarthria) and loss of volume (dysphonia) occur in approximately 25-40% of people with MS, particularly later in the disease course and during periods of extreme fatigue. Stuttering is occasionally reported as well.
*Swallowing problems — referred to as dysphagia — result from damage to the nerves controlling the many small muscles in the mouth and throat.
*Tremor, or uncontrollable shaking, can occur in various parts of the body because of damaged areas along the complex nerve pathways that are responsible for coordination of movements.
*Seizures — which are the result of abnormal electrical discharges in an injured or scarred area of the brain — have been estimated to occur in 2-5% people with MS, compared to the estimated 3% of the general population.
*Breathing Problems-Respiration problems occur in people whose chest muscles have been severely weakened by damage to the nerves that control those muscles.
*Itching-Pruritis (itching) is one of the family of abnormal sensations — such as “pins and needles” and burning, stabbing or tearing pains — which may be experienced by people with MS.
*Headaches-Although headache is not a common symptom of MS, some reports suggest that people with MS have an increased incidence of certain types of headache.
*Hearing Loss-About 6% of people who have MS complain of impaired hearing. In very rare cases, hearing loss has been reported as the first symptom of the disease.
Stayed tune Part III in modern treatments with Types of Multiple Sclerosis tomorrow!
Updated 3/16/2023