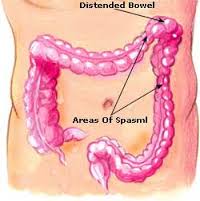
Irritable bowel syndrome is a group of symptoms – including abdominal pain and changes in the pattern of bowel movements without any evidence of underlying damage. These symptoms occur over a long time, often years. It has been classified into four main types depending on if diarrhea is common, constipation is common, both are common, or neither occurs very often. IBS negatively affects quality of life and may result in missed school or work. Disorders such as anxiety, major depression, and chronic fatigue syndrome, are common among people with IBS.
Treatments and drugs
Because it’s not clear what causes irritable bowel syndrome, treatment focuses on the relief of symptoms so that you can live as normally as possible.
In most cases, you can successfully control mild signs and symptoms of irritable bowel syndrome by learning to manage stress and making changes in your diet and lifestyle. Try to avoid foods that trigger your symptoms. Also try to get enough exercise, drink plenty of fluids and get enough sleep.
If your problems are moderate or severe, you may need more than lifestyle changes. Your doctor may suggest medications.
Dietary changes:
- Eliminating high-gas foods. If you have bothersome bloating or are passing considerable amounts of gas, your doctor may suggest that you cut out such items as carbonated beverages, vegetables — especially cabbage, broccoli and cauliflower — and raw fruits.
- Eliminating gluten. Research shows that some people with IBS report improvement in diarrhea symptoms if they stop eating gluten (wheat, barley and rye). This recommendation remains controversial, and the evidence is not clear.
- Eliminating FODMAPs. Some people are sensitive to types of carbohydrates such as fructose, fructans, lactose and others, called FODMAPs (fermentable oligo-, di-, and monosaccharides and polyols). FODMAPs are found in certain grains, vegetables, fruits and dairy products. However, often people are not bothered by every FODMAP food. You may be able to get relief from your IBS symptoms on a strict low FODMAP diet and then reintroduce foods one at time.
- Medications:
- Fiber supplements. Taking fiber supplements, such as psyllium (Metamucil) or methylcellulose (Citrucel), with fluids may help control constipation. Fiber obtained from food may cause much more bloating compared with a fiber supplement. If fiber doesn’t help symptoms, your doctor may prescribe an osmotic laxative such as milk of magnesia or polyethylene glycol.
- Anti-diarrheal medications. Over-the-counter medications, such as loperamide (Imodium), can help control diarrhea. Some people will benefit from medications called bile acid binders, such as cholestyramine (Prevalite), colestipol (Colestid) or colesevelam (Welchol), but these can lead to bloating.
- Anticholinergic and antispasmodic medications. These medications, such as hyoscyamine (Levsin) and dicyclomine (Bentyl), can help relieve painful bowel spasms. They are sometimes used for people who have bouts of diarrhea, but they can worsen constipation and can lead to other symptoms, such as difficulty urinating. They should also be used with caution among people with glaucoma.
- Antidepressant medications. If your symptoms include pain or depression, your doctor may recommend a tricyclic antidepressant or a selective serotonin reuptake inhibitor (SSRI). These medications help relieve depression as well as inhibit the activity of neurons that control the intestines.
- If you have diarrhea and abdominal pain without depression, your doctor may suggest a lower than normal dose of tricyclic antidepressants, such as imipramine (Tofranil) or nortriptyline (Pamelor). Side effects of these drugs include drowsiness and constipation. SSRIs, such as fluoxetine (Prozac, Sarafem) or paroxetine (Paxil), may be helpful if you’re depressed and have pain and constipation.
- Antibiotics. Some people whose symptoms are due to an overgrowth of bacteria in their intestines may benefit from antibiotic treatment. Some people with symptoms of diarrhea have benefited from rifaximin (Xifaxan), but more research is needed.
- Counseling. You may benefit from counseling if you have depression or if stress tends to worsen your symptoms. Two medications are currently approved for specific cases of IBS:
- Medication specifically for IBS
- Alosetron (Lotronex). Alosetron is designed to relax the colon and slow the movement of waste through the lower bowel. The Food and Drug Administration (FDA) removed it from the market for a time, but has since allowed alosetron to be sold again.
- However, alosetron can be prescribed only by doctors enrolled in a special program and is intended for severe cases of diarrhea-predominant IBS in women who haven’t responded to other treatments. Alosetron is not approved for use by men. It has been linked to rare but important side effects, so it should only be considered when other treatments are not successful.
- Lubiprostone (Amitiza). Lubiprostone works by increasing fluid secretion in your small intestine to help with the passage of stool. It is approved for women age 18 and older who have IBS with constipation. Its effectiveness in men is not proved, nor its long-term safety. Common side effects include nausea, diarrhea and abdominal pain. Lubiprostone is generally prescribed only for women with IBS and severe constipation for whom other treatments haven’t been successful.