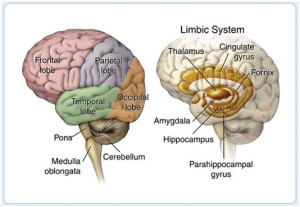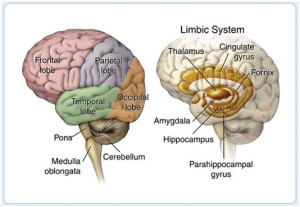
An acquired brain injury (ABI) is an injury to the brain that is not hereditary, congenital, degenerative, or induced by birth trauma. Essentially, this type of brain injury is one that has occurred after birth. The injury results in a change to the brain’s neuronal activity, which affects the physical integrity, metabolic activity, or functional ability of nerve cells in the brain.
There are two types of acquired brain injury: traumatic and non-traumatic.
A traumatic brain injury (TBI) is defined as an alteration in brain function, or other evidence of brain pathology, caused by an external force. Traumatic impact injuries can be defined as closed (or non-penetrating) or open (penetrating).
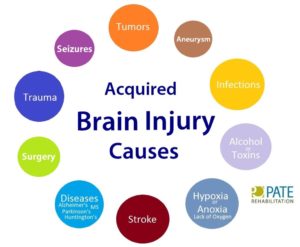
Often referred to as an acquired brain injury, a non-traumatic brain injury causes damage to the brain by internal factors, such as a lack of oxygen, exposure to toxins, pressure from a tumor, etc.
A Brain Injury is damage to the brain that results in a loss of function such as mobility or feeling.
Traumatic Brain Injuries can result from a closed head injury or a penetrating head injury.
Closed Injury: A closed injury occurs when the head suddenly and violently hits an object but the object does not break through the skull.
Penetrating Injury: A penetrating injury occurs when an object pierces the skull and enters brain tissue. As the first line of defense, the skull is particularly vulnerable to injury. Skull fractures occur when the bone of the skull cracks or breaks. A depressed skull fracture occurs when pieces of the broken skull press into the tissue of the brain. A penetrating skull fracture occurs when something pierces the skull, such as a bullet, leaving a distinct and localized injury to brain tissue. Skull fractures can cause cerebral contusion.
Brain trauma occurs when a person has an injury to the brain, and can be mild or severe. When a person sustains trauma to the brain, he or she may lose motor functions along with cognitive and physical abilities. Physicians use the Glasgow Coma Scale to determine the extent of brain trauma. This is a neurological scale that measures the level of a person’s consciousness. The Rancho Los Amigos Scale is used to monitor the recovery of the brain.
There are several different types of brain injuries. A mild injury may cause temporary symptoms while a severe injury could require years of rehabilitation. The two most common types of brain trauma are:
1. Traumatic Brain Injuries
2. Acquired Brain Injuries.
1-Traumatic brain injury occurs from external force on the head or neck. These injuries can occur from blows to the head or aggressive twisting of the neck. Some ways this could happen include falls, motor vehicle accidents, sports, and vigorous shaking. In infants, Shaken Baby Syndrome is a type of traumatic brain injury.
2-An acquired brain injury means simply you got this injury after you were born and it was caused by a condition or illness after birth. This type of injury can result from several different causes like strokes, toxic poisoning or brain tumors. Degenerative diseases and lack of oxygen may also cause this type of brain trauma. Here are some examples of acquired brain injuries:
-Bleeding in the brain which can lead to brain injury. Blood Vessels in the brain can rupture resulting in an intra-cerebral hemorrhagic (one of the causes of a stroke, its what we called Hemorrhagic Stroke). Symptoms may include headaches, loss of vision, weakness to one side of the body and eye pain to even garbled speech.
Other Causes of Brian Injury:
-Anoxia is another insult to the brain that can cause injury. Anoxia is a condition in which there is an absence of oxygen supply to an organ’s tissues, even if there is adequate blood flow to the tissue. Common causes of anoxia are near drowning, choking, suffocation, strangulation, heart attacks, lung damage, or very low blood pressure. They all decrease oxygen intake to the red blood cells that feed the organs nutrients (being oxygen) to our body. Anoxia is starvation to our body tissues.
-Hypoxia:
Hypoxia refers to a decrease in oxygen supply rather than a complete absence of oxygen, and ischemia is inadequate blood supply, as is seen in cases in which the brain swells that causes compressing on the brain vessels near where the swelling is. In any of these cases, without adequate oxygen, a biochemical cascade called the ischemic cascade is unleashed, and the cells of the brain can die within several minutes. This type of injury is often seen in near-drowning victims, in heart attack patients, or in people who suffer significant blood loss from other injuries that decrease blood flow to the brain.
-Toxemia:
This occurs due to poisoning from chemical or biological factors that can damage the brain. Toxemia can be caused by drugs, chemicals, gases or even toxic foods.
-Viruses and bacteria. An infection of the brain can be very damaging like:
*Meningitis is a inflammation of the lining around the brain or spinal cord, usually due to infection; Neck stiffness, headache, fever, and confusion are common symptoms.
*Encephalitis (en-sef-uh-LIE-tis) is inflammation of the brain. Viral infections are the most common cause of the condition. Encephalitis can cause flu-like symptoms, such as a fever or severe headache. It can also cause confused thinking, seizures, or problems with senses or movement.
*HIV can lead to brain injury. HIV, can affect the brain in different ways. HIV-meningoencephalitis is infection of the brain and the lining of the brain by the HIV virus. It occurs shortly after the person is first infected with HIV and may cause headache, neck stiffness, drowsiness, confusion and/or seizures. HIV-encephalopathy (HIV-associated dementia) is the result of damage to the brain by longstanding HIV infection. It is a form of dementia and occurs in advanced HIV infection. Mild Neurocognitive Disorder is problems with thinking and memory in HIV, however is not as severe as HIV-encephalopathy. Unlike HIV-encephalopathy it can occur early in HIV infection and is not a feature of Aquired Immune Deficiency Syndrome – AIDS.
*Lastly, Herpes. There are two types of herpes simplex virus (HSV). Either type can cause encephalitis. HSV type 1 (HSV-1) is usually responsible for cold sores or fever blisters around your mouth, and HSV type 2 (HSV-2) commonly causes genital herpes. Encephalitis caused by HSV-1 is rare, but it has the potential to cause significant brain damage or death.
*Other herpes viruses. Other herpes viruses that may cause encephalitis include the Epstein-Barr virus, which commonly causes infectious mononucleosis, and the varicella-zoster virus, which commonly causes chickenpox and shingles.*Viral infections due to blood sucking insects like mosquitoes and ticks to animals with rabies a rapid progression to encephalitis once symptoms begin. Rabies is a rare cause of encephalitis in the U.S.
When a person is diagnosed with a brain trauma, doctors will decide if rehabilitation is needed.
Rehabilitation programs may vary depending on the type of brain injury and estimated recovery time. Treatment usually consists of physical therapy and daily activities. In extreme cases, patients may need to learn how to read and write again.
Therapy for brain trauma typically takes place on an outpatient basis or through an assisted living facility. Therapy may last several weeks, months or even years, and sometimes the patient is not able to make a full recovery.
It may not always be obvious when a person has sustained a brain injury. The patient may have hit his or her head and not have symptoms until a few hours later. Some signs of a possible brain injury are headaches, confusion and loss of memory. If brain trauma is not treated, it could cause permanent damage or death.
Brain injuries can affect the patient and the patient’s family, with emotional and financial hardship. When problems arise with treatment or financial issues, a brain injury lawyer or specialist may need to intervene.
REVISED 2/25/2021 By Elizabeth Lynch RN BSN Cardiac/Stroke Certified (RN 34.5 Years)