Well check out about White Meat vs. Red Meat:
1-White Meat
White meat is best known as meat that is lean, especially in comparison with red meat. The big point about white meat is that its fat content is less in comparison with red meat. Meats traditionally thought of as white (such as veal and even lamb) have been reclassified as red meats. Another advantage to eating white meat over red meat, which is also why health experts recommend it over red meat, is the lower number of calories that it contains. However, the difference in calories between white meat and red meat is not so great that it will absolutely ruin your waistline if you choose to eat some red meat once in a while.
2-Red Meat
Red meat is the victim of stereotypes that have been exaggerated to the point where it is today somewhat stigmatized as a food that is linked to cancer and higher fat and caloric content. While the cancer issue depends on what studies you look at and the higher caloric content is not that much over white meat, red meat does have benefits that white meat simply lacks. For example, the nutrients zinc, iron, thiamine and riboflavin (in addition to vitamins B12 and B6) appear in much greater abundance in red meat. Moreover, red meat is a great source of muscle-building protein as well as being the best source of the antioxidant called alpha lipoic acid. Still, red meat has been the subject of a lot of studies that connect it to health problems beyond cancer, like cardiovascular disease and even arthritis and hypertension.
Which One to Choose:
The bottom line is that no matter which meat you eat, you can guard yourself against health problems if you eat in moderation. While white meat is not tied to as many health problems as red meat is, it does not feature many of the benefits that you get in red meat, such as the vitamins and minerals. So if you want to get a dose of said nutrients, you should eat more red meat, but do so in a way that is only moderate
HERE IS SOME FACTS ABOUT TURKEY:
Because most cuts of turkey provide valuable amounts of protein, turkey is often regarded as a high-protein food. Skinned turkey breast will provide the most protein per serving, at 34 grams in 4 ounces. But you will still get 31 grams from 4 ounces of turkey leg and 21 grams from 4 ounces of turkey thigh.
In addition to protein, however, turkey is also rich in other nutrients. All B vitamins are present in turkey meat, including B1, B2, B3, B5, B6, B12, folate, biotin, and choline. (Because the biotin content of turkey meat is sensitive to the turkey’s dietary intake, the amount of this vitamin can vary greatly, with an approximate average of 0.8 micrograms in 4 ounces of turkey breast.) Turkey is a very good source for vitamin B3 and provides about 8.5 milligram in 4 ounces, or over 40% of the Daily Value (DV). It’s also a very good source of vitamin B6, at 0.64 milligrams in 4 ounces (32% DV). By providing 22%DV for choline in 4 ounces, turkey also ranks as a good source of this B vitamin.
In terms of minerals, turkey is richest in selenium and provides over 50% of the DV in a single 4-ounce serving. Zinc, copper, phosphorus, magnesium, potassium, and iron are also provided by this food in amounts varying from 5-15% DV.
All cuts of turkey contain omega-3 fats. However, the content of omega-3s in turkey can vary widely, depending on the turkey’s diet. One of the reasons we recommend pasture-raised turkey is the ability of turkeys to enjoy omega-3 containing plants and insects in natural pasture settings. As a general rule, the most favorable ratio of omega-6 to omega-3 fats is found in skinned turkey breast, where the ratio in non-pasture-raised turkey is approximately 10:1. This same ratio is about 13:1 in non-pasture-raised turkey leg or turkey thigh with skin. While there are only a few studies documenting the omega-6 to omega-3 ratio in pasture-raised turkey, those studies suggest that pasture feeding can lower the ratio to approximately 7:1. (There are some studies on pasture-raised chickens that show similar results.) Within the omega-3 family of fats, it is possible to get 10-60 milligrams of DHA (docosahexaenoic acid) from a 4-ounce serving of turkey, depending on the cut and diet consumed by the turkey. DHA is a unique omega-3 fat in terms of its ability to support healthy nerve function.
Protein Richness
When we rank all of our 100+ WHFoods based on their protein richness (how much protein they provide in comparison with their calorie content), turkey ranks first among all of our foods. A 4-ounce serving of skinned baked turkey breast provides about 34 grams of protein and over two-thirds of the Daily Value (DV). With 4 ounces of turkey leg, this number drops just slightly to 31-32 grams of protein. With 4 ounces of turkey thigh, it drops to about 21 grams. In these examples, the protein values are changing from cut-to-cut partly because of the way the turkey moves and uses its muscles, and partly because of the fat content of the various cuts. If the health benefit you are seeking from turkey is focused on protein richness, you’ll probably want to stick with skinned turkey breast as your preferred cut.
Other Health Benefits
Unfortunately, there is not as much research on turkey as there is on chicken, its fellow bird in the poultry category. Several preliminary studies show the protein richness of turkey to be of potential benefit in regulating blood sugar levels as well as insulin metabolism. These findings make sense since adequate protein intake in a balanced way throughout the day can be very helpful in managing blood sugar. In the area of cancer prevention, turkey shows that intake of it is not associated with increased cancer risk in the same way as red meats. However,they simply show that turkey intake does not raise this risk which is still a plus compared to some other foods.
Description
Like chicken, turkey belongs to the bird (Aves) class of animals, and to the family of birds called Phasianidae. While there are many different breeds of turkeys, most of them belong to the same genus and species of bird, namely Meleagris gallopavo. Turkeys are truly native to North and South America – they were not brought to the “New World” by European settlers but were instead discovered to be already present and intimately involved with Native American cultures. Turkeys are relatively large birds that can reach about 30-35 pounds in weight. They can fly short distances at speeds of about 50-55 miles per hour and run at approximately 20-25 miles per hour.
History:
At 2.5 million tons of turkey meat per year, the U.S. is by far the world’s largest producer of turkey. (All countries in the European Union combined produce 1.75 million tons.) Smaller amounts of turkey are produced in Africa, Asia, and the Mediterranean. At about 450,000 tons, Brazil is the largest turkey producer in South America.
In the U.S., we consume an average of 16.5 pounds of turkey per person per year. That about is about one-quarter of our chicken consumption.
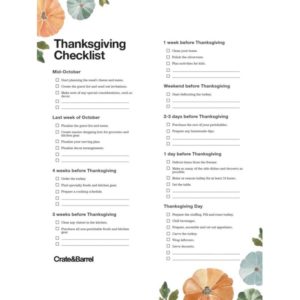
According to the National Turkey Federation, about 20% of all turkey (just over three pounds per person) is consumed on Thanksgiving Day, Gobble Gobble Day.
How to Select and Store:
It’s worth taking special care in the selection of turkey! Several aspects of turkey selection will help you maximize your health benefits from this World’s Healthiest Food. First, we recommend the purchase of fresh turkey. Technically, the U.S. Department of Agriculture (USDA) guidelines allow use of the word “fresh” only when turkey has never been stored a temperature below 26°F (-3°C). (Otherwise, the term “frozen” or “previously frozen” would be required.) Additives like sodium erythorbate, MSG, and salt are not allowed on fresh turkey, and that’s a major health advantage for you.